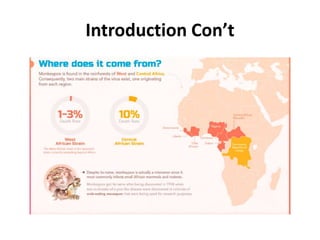
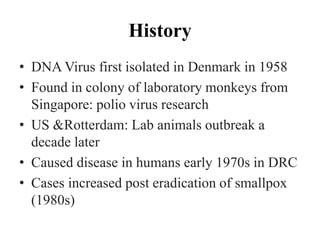
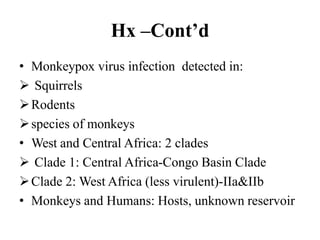
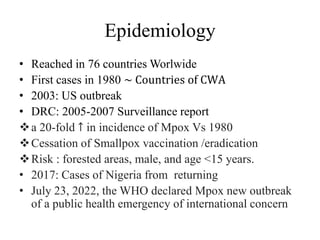
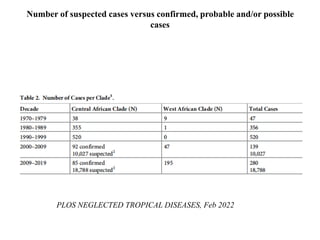
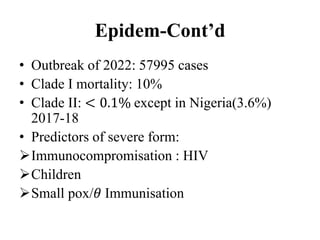
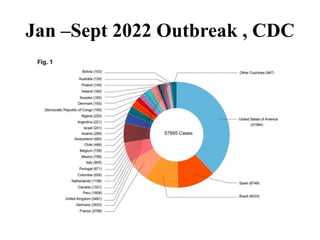
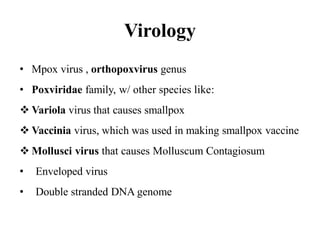
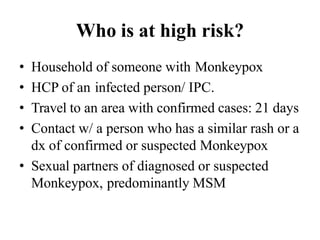
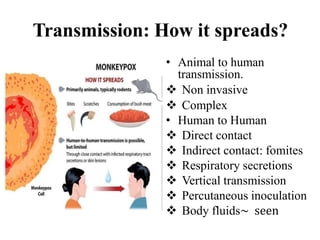
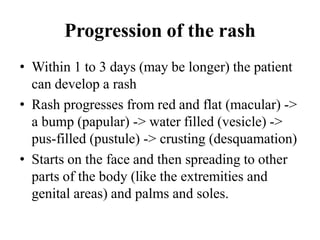
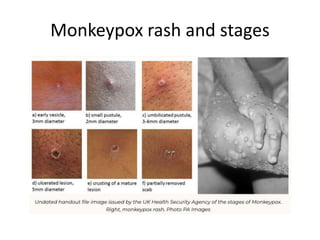
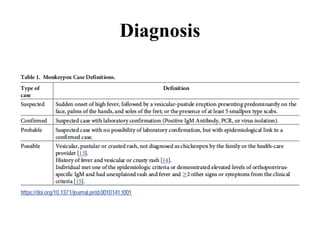
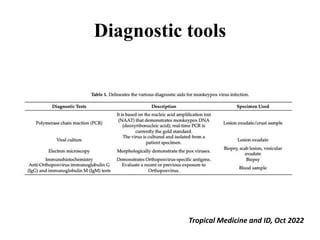
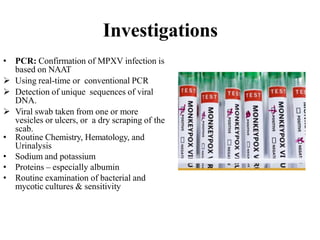
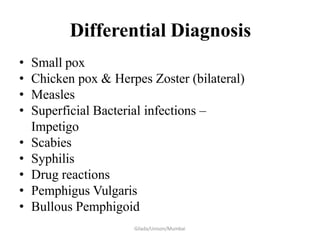
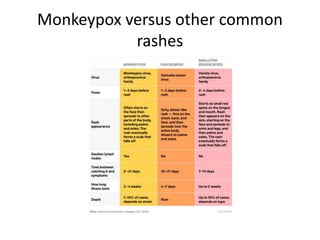
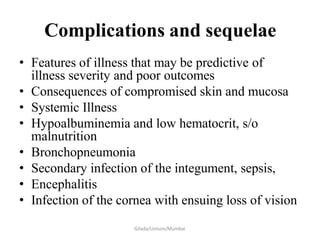
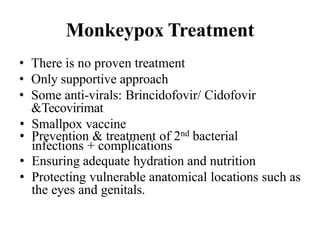
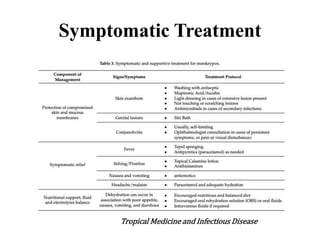
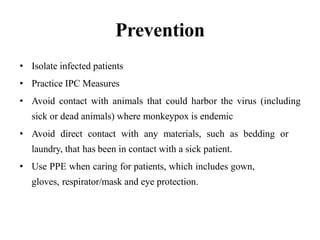
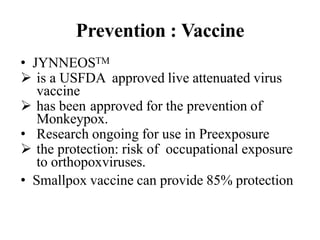
Monkeypox is a zoonotic virus that presents with a rash similar to smallpox. It is endemic to parts of Central and West Africa. The current outbreak has spread to over 70 countries. Transmission occurs through direct contact with lesions, droplets, or fomites. Symptoms include fever, headache, and a rash that starts on the face and spreads. Diagnosis is via PCR testing of lesions. Treatment is supportive with antivirals being studied. Prevention includes isolation, PPE, vaccination, and avoiding contact with sick animals in endemic regions.