This document provides an overview of ulnar nerve injury, including:
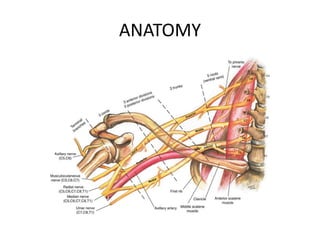
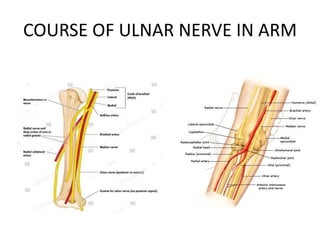
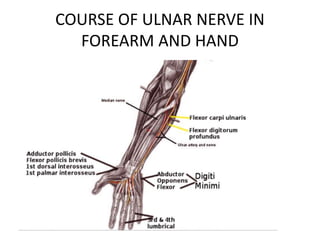
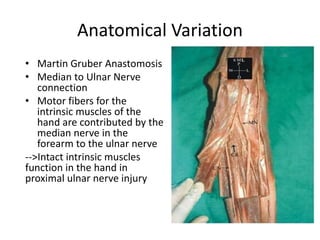
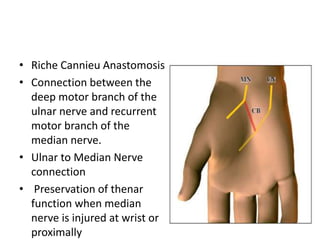
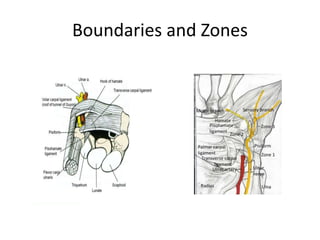
- Anatomy of the ulnar nerve and the muscles it innervates
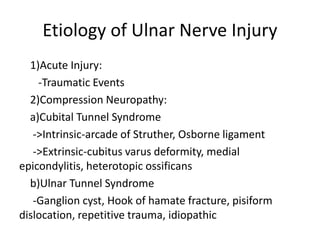
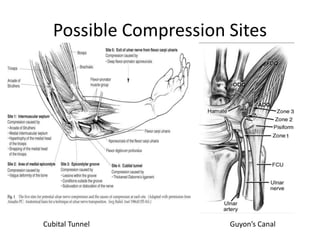
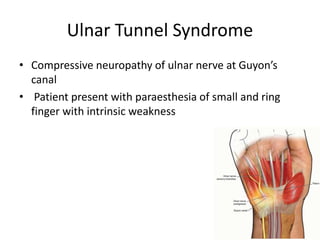
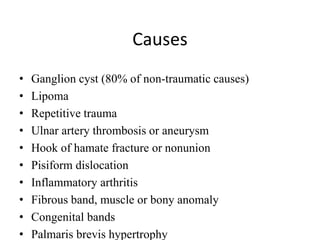
- Common causes of ulnar nerve injury such as trauma, compression neuropathies like cubital tunnel syndrome
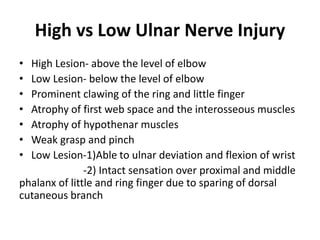
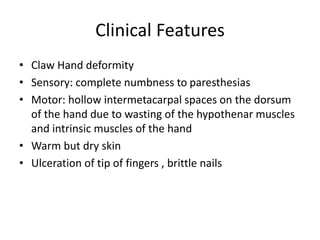
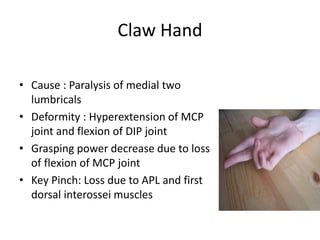
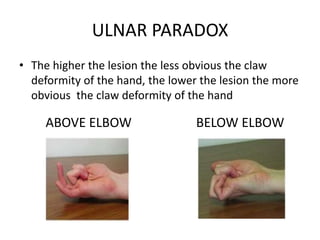
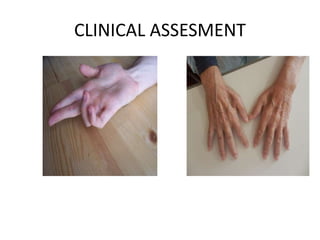
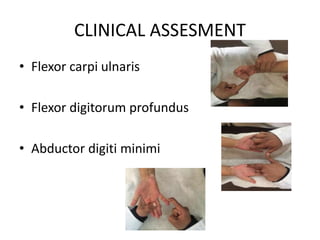
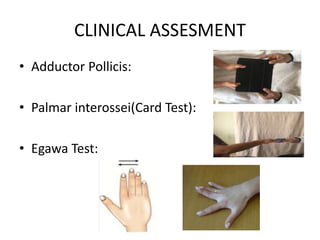
- Clinical signs of ulnar nerve injury including clawing of the ring and little fingers
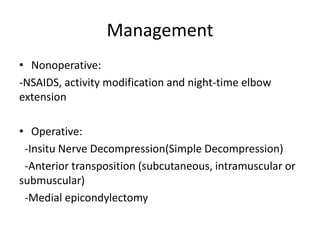
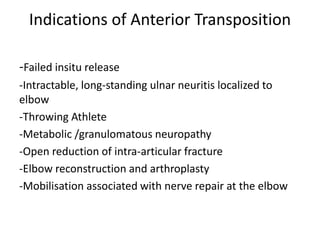
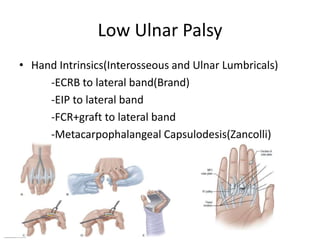
- Surgical management options like nerve repair, grafting, decompression for compression neuropathies, and tendon transfers to restore hand function
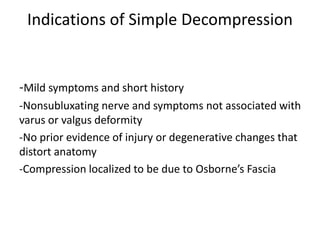
- Specific procedures for cubital tunnel syndrome and ulnar tunnel syndrome decompression