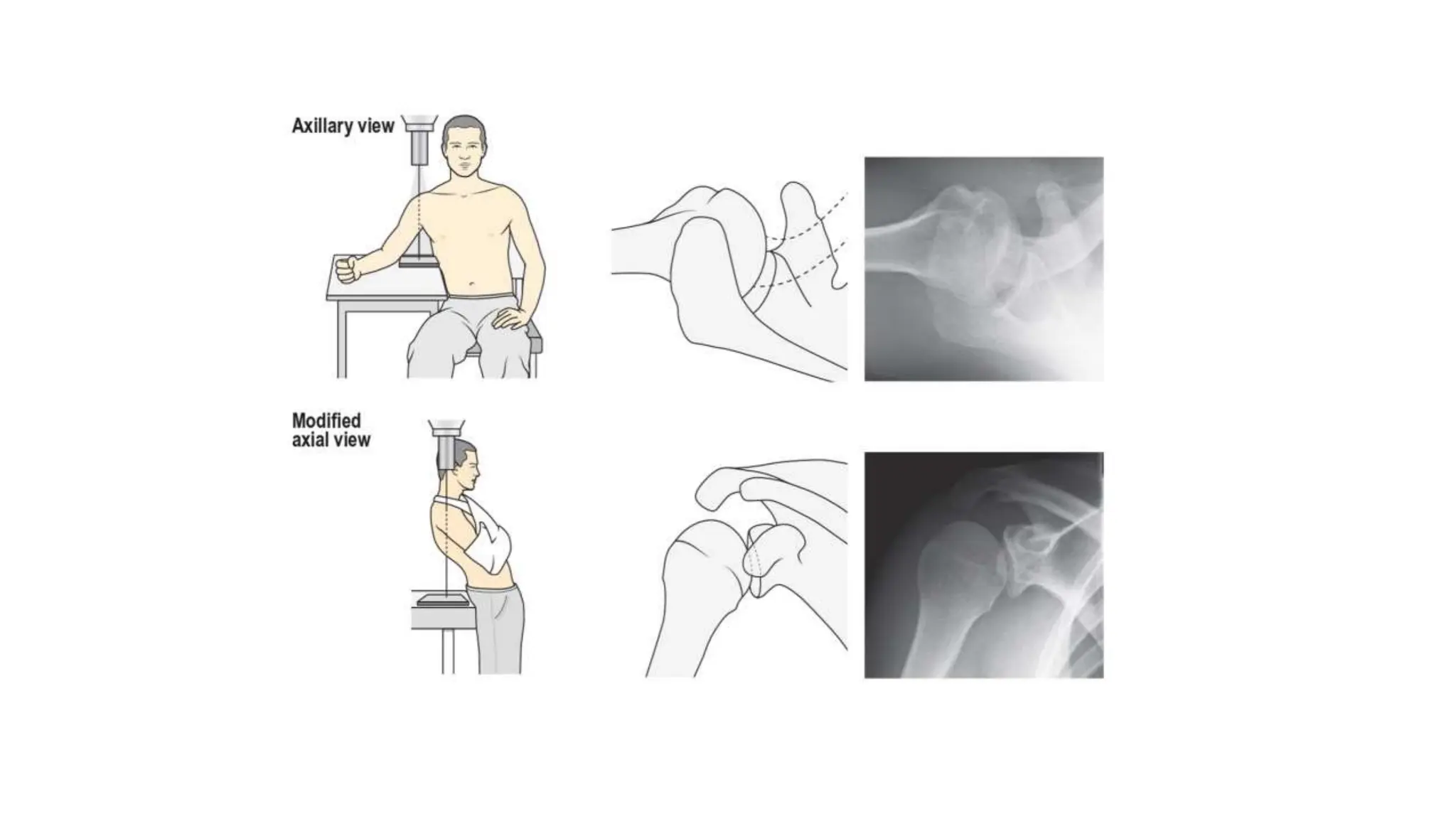
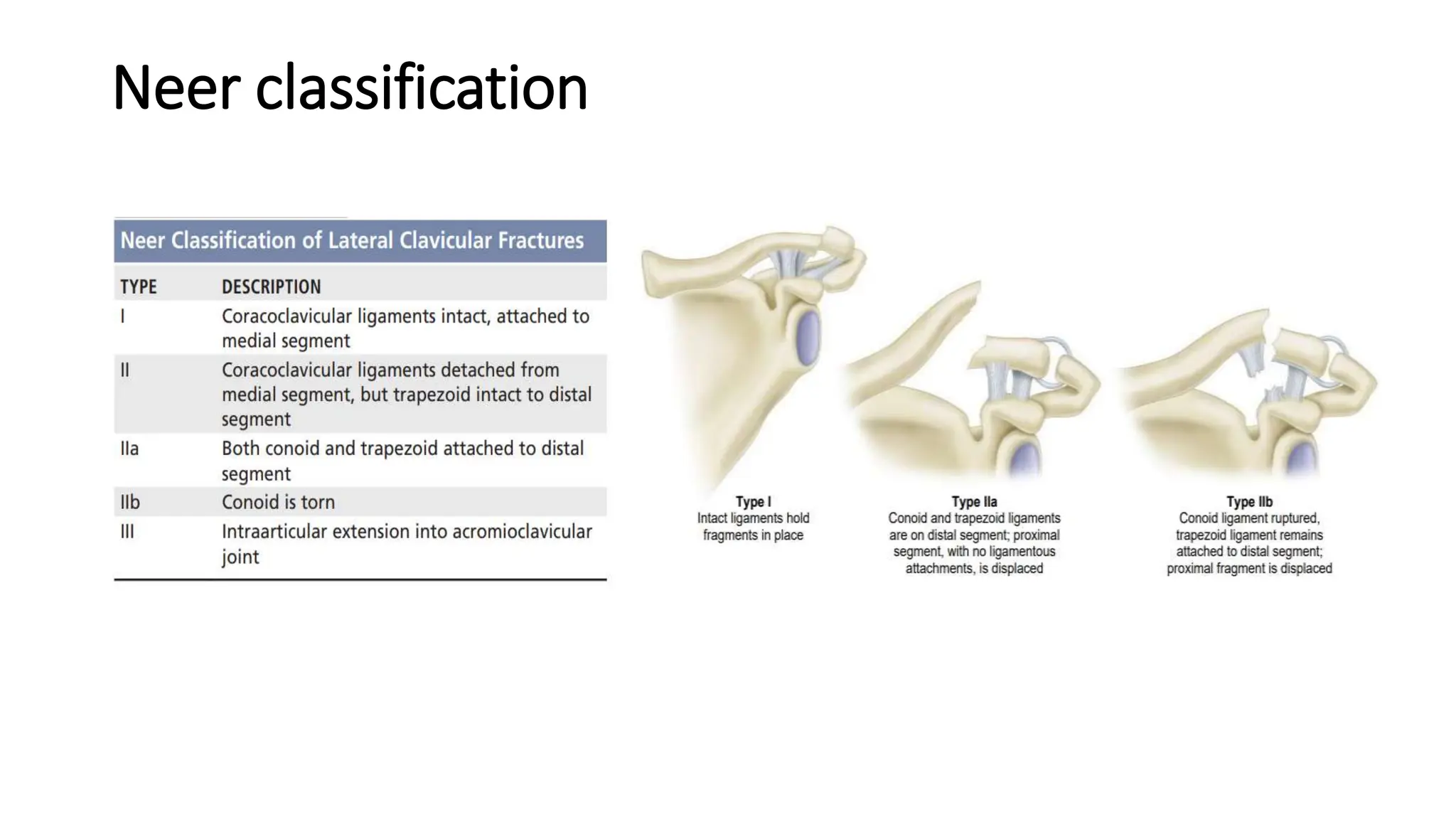
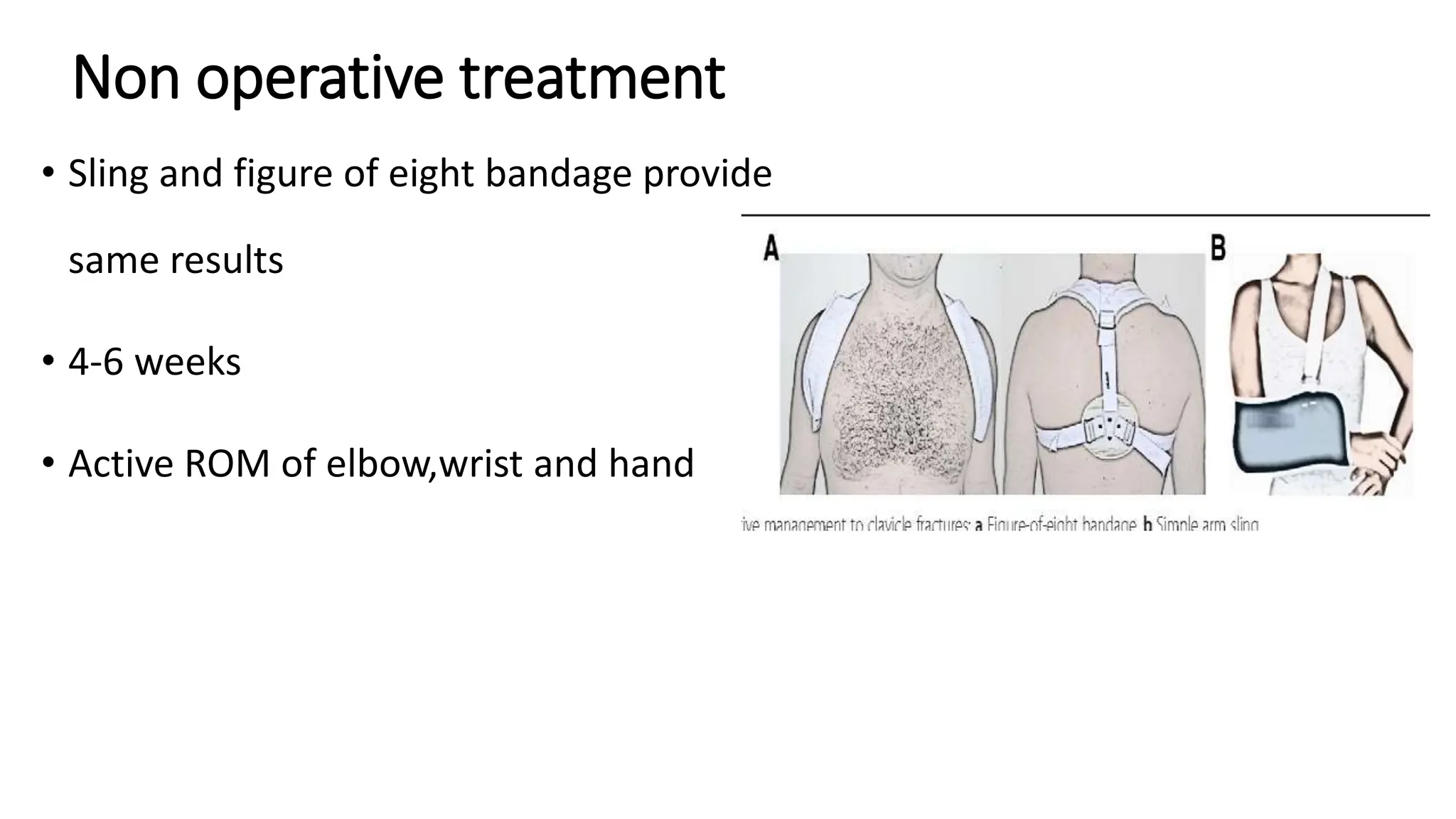
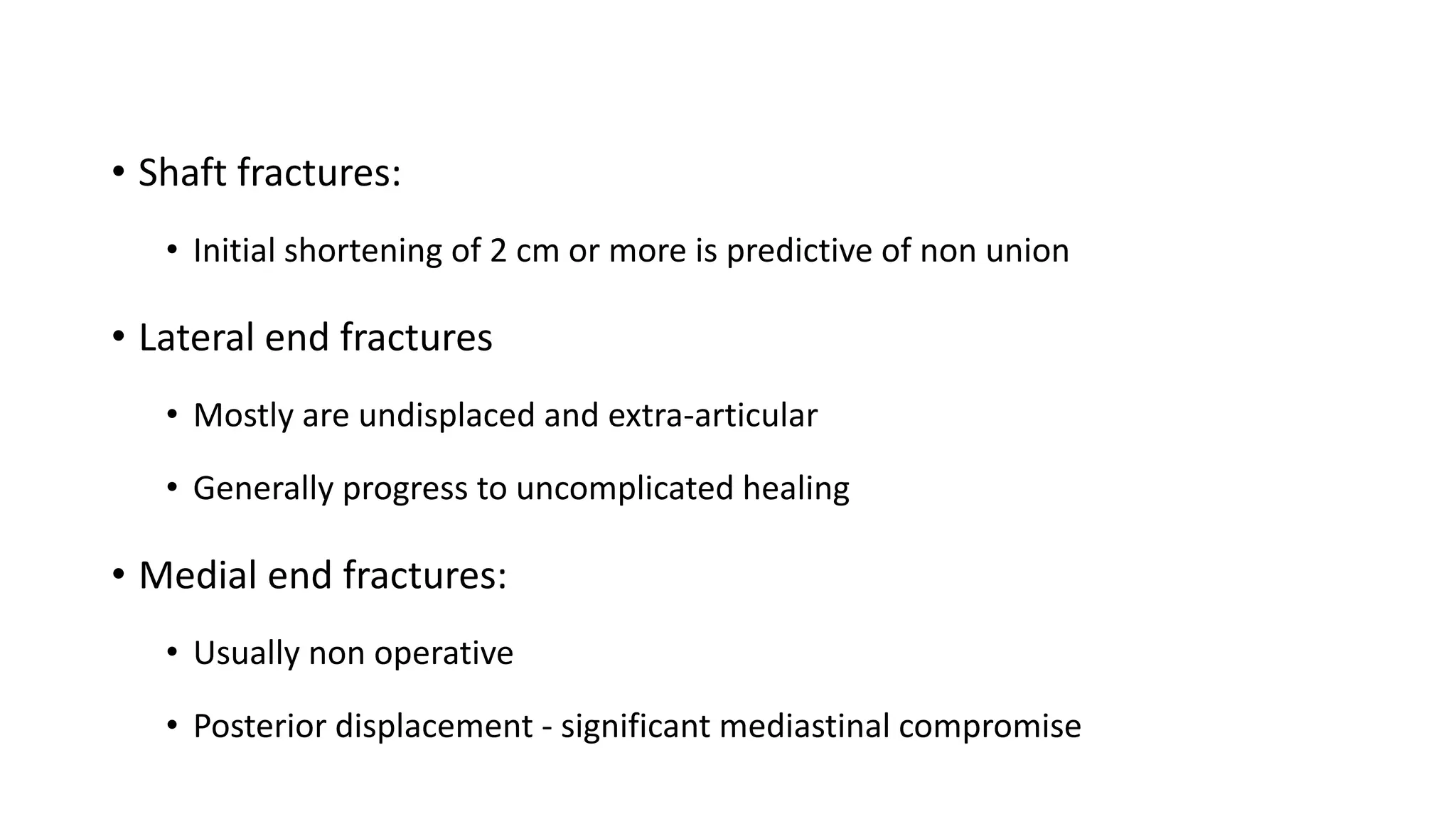
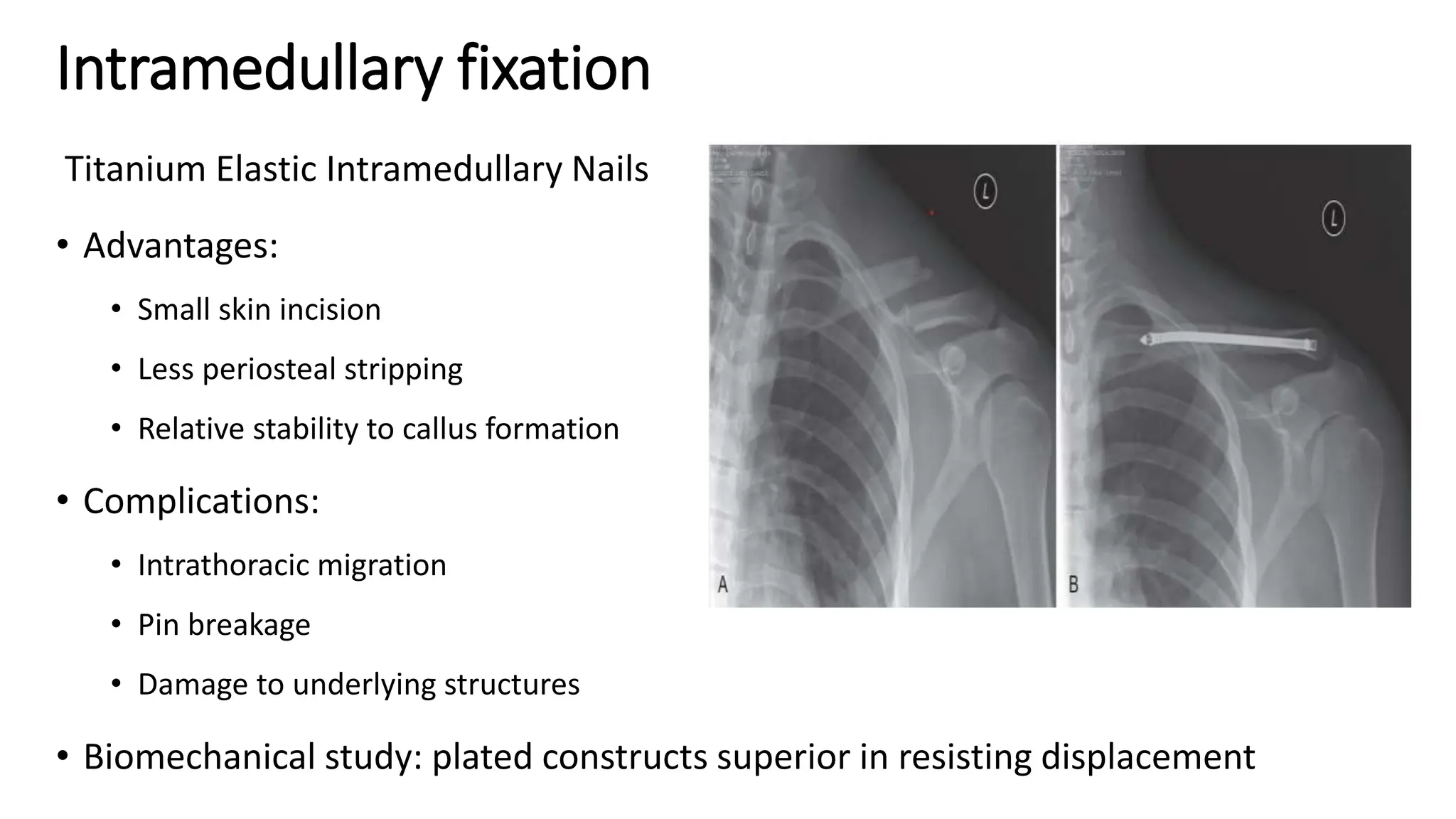
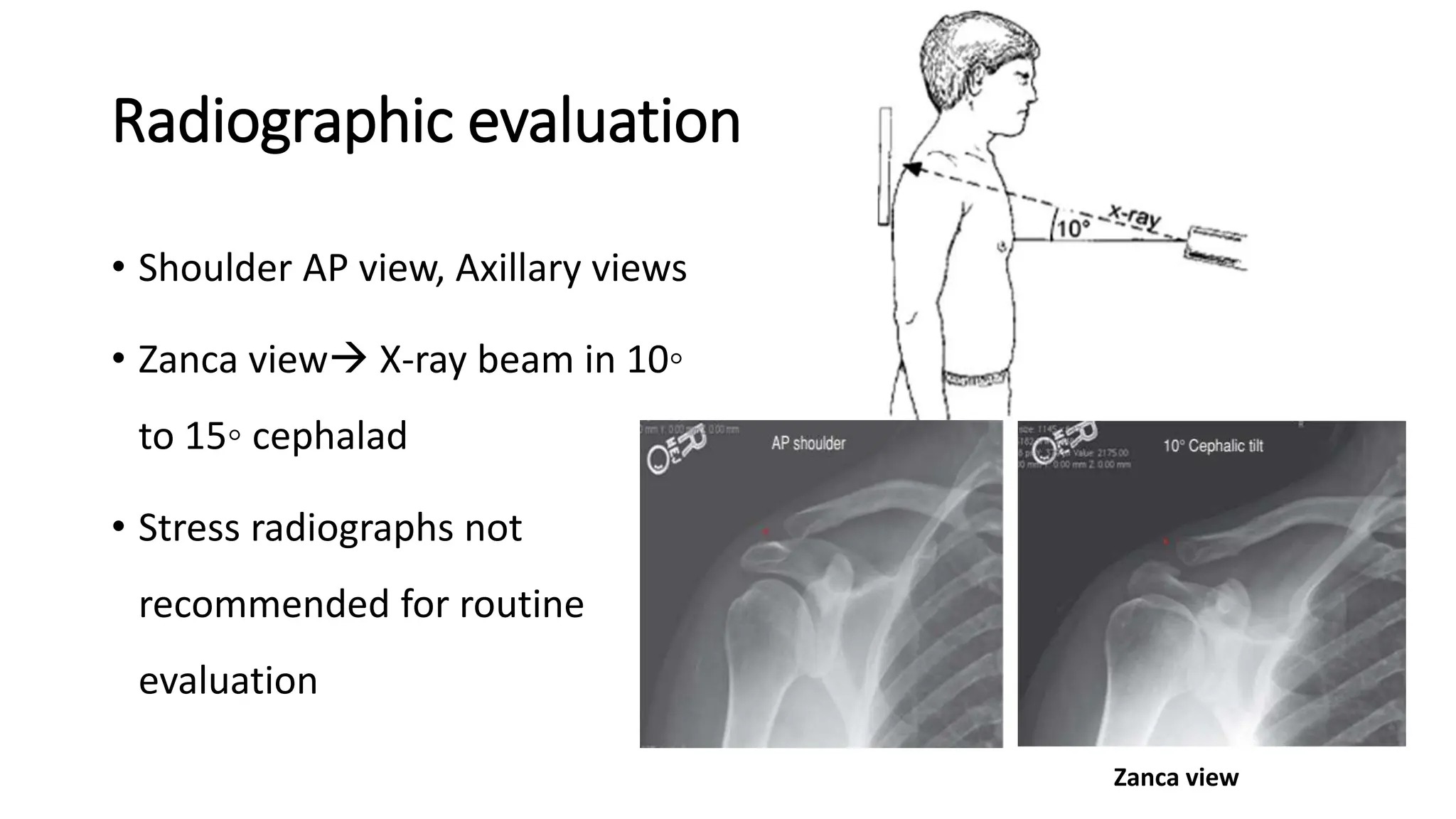
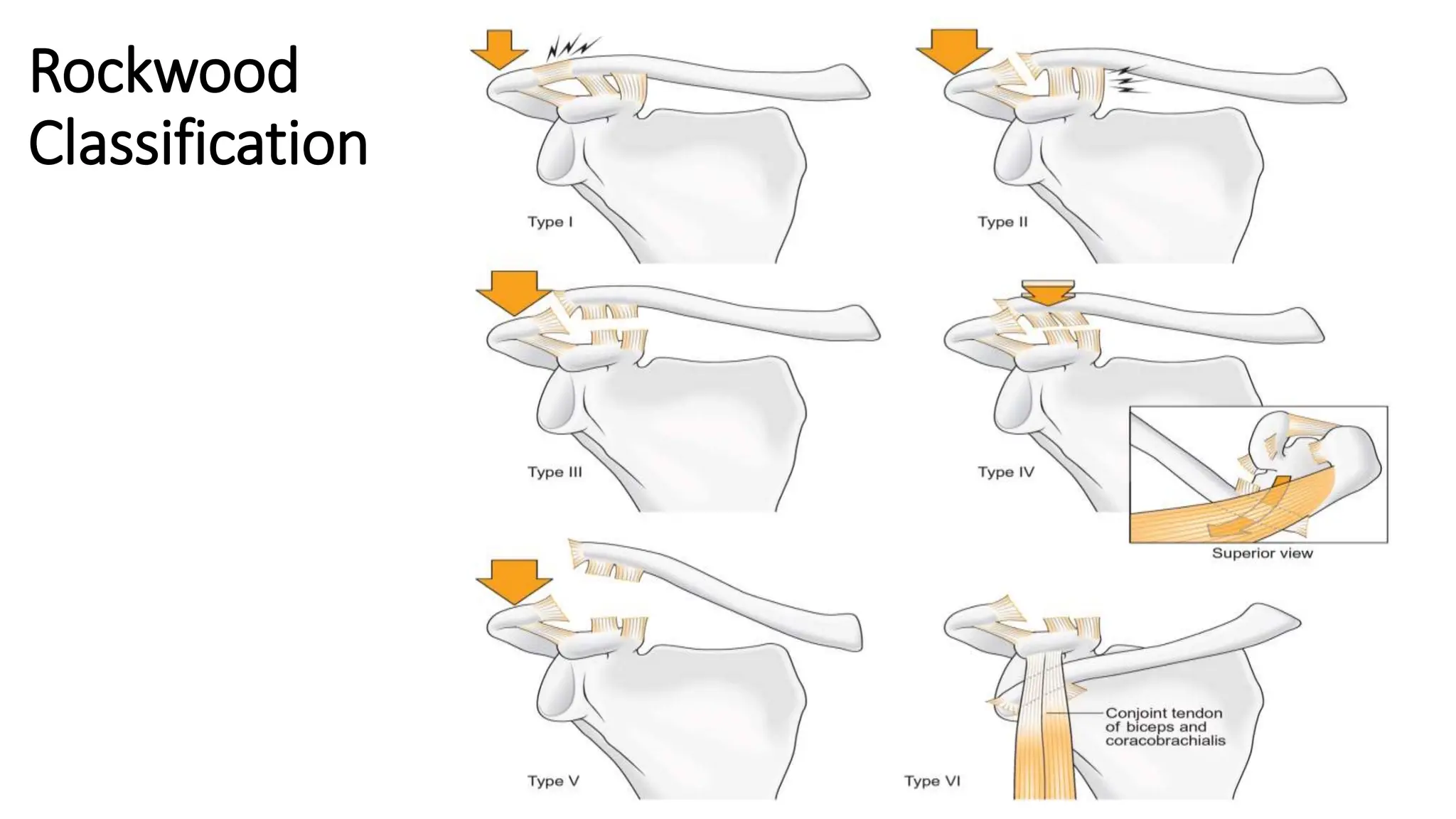
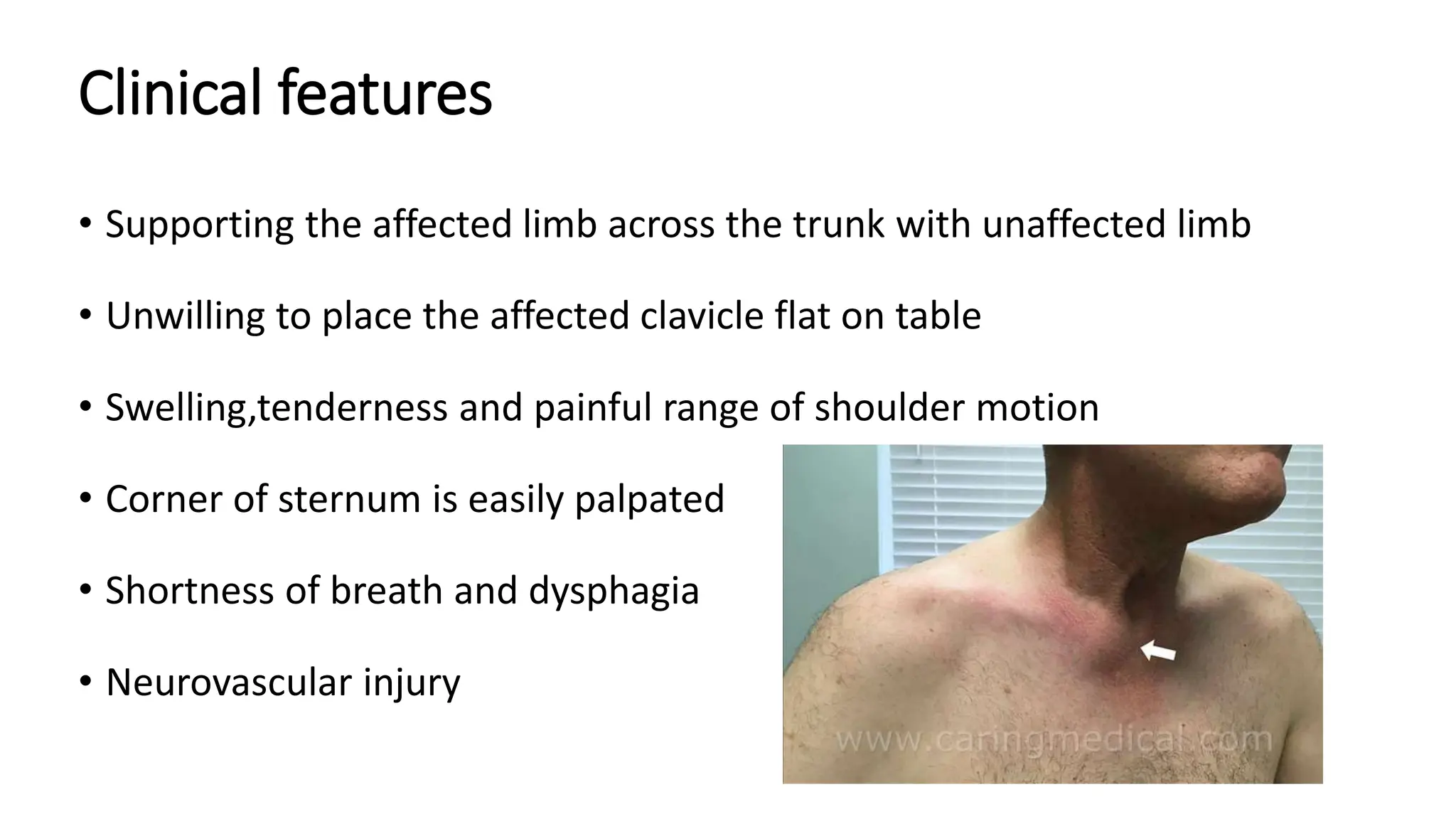
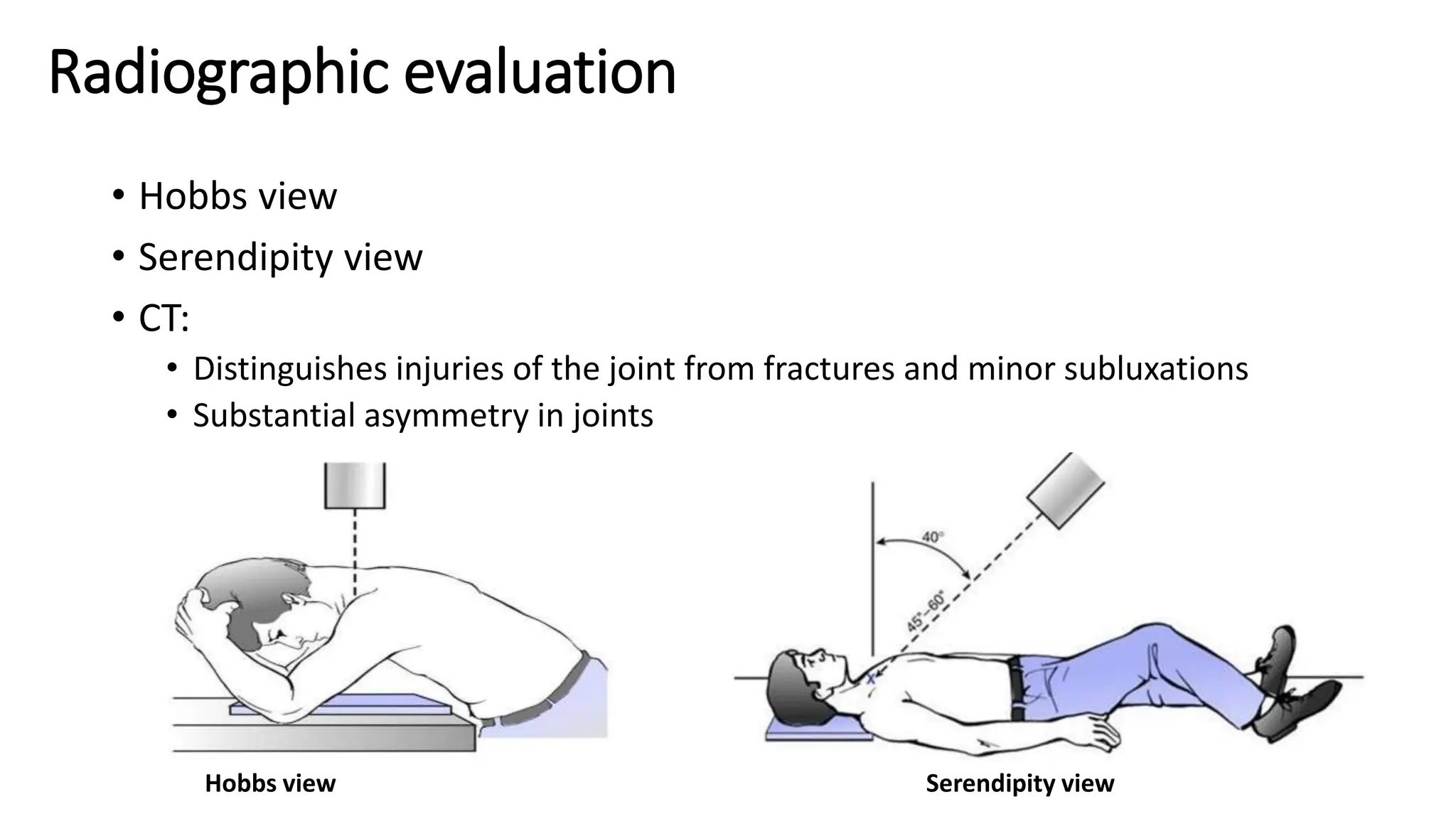
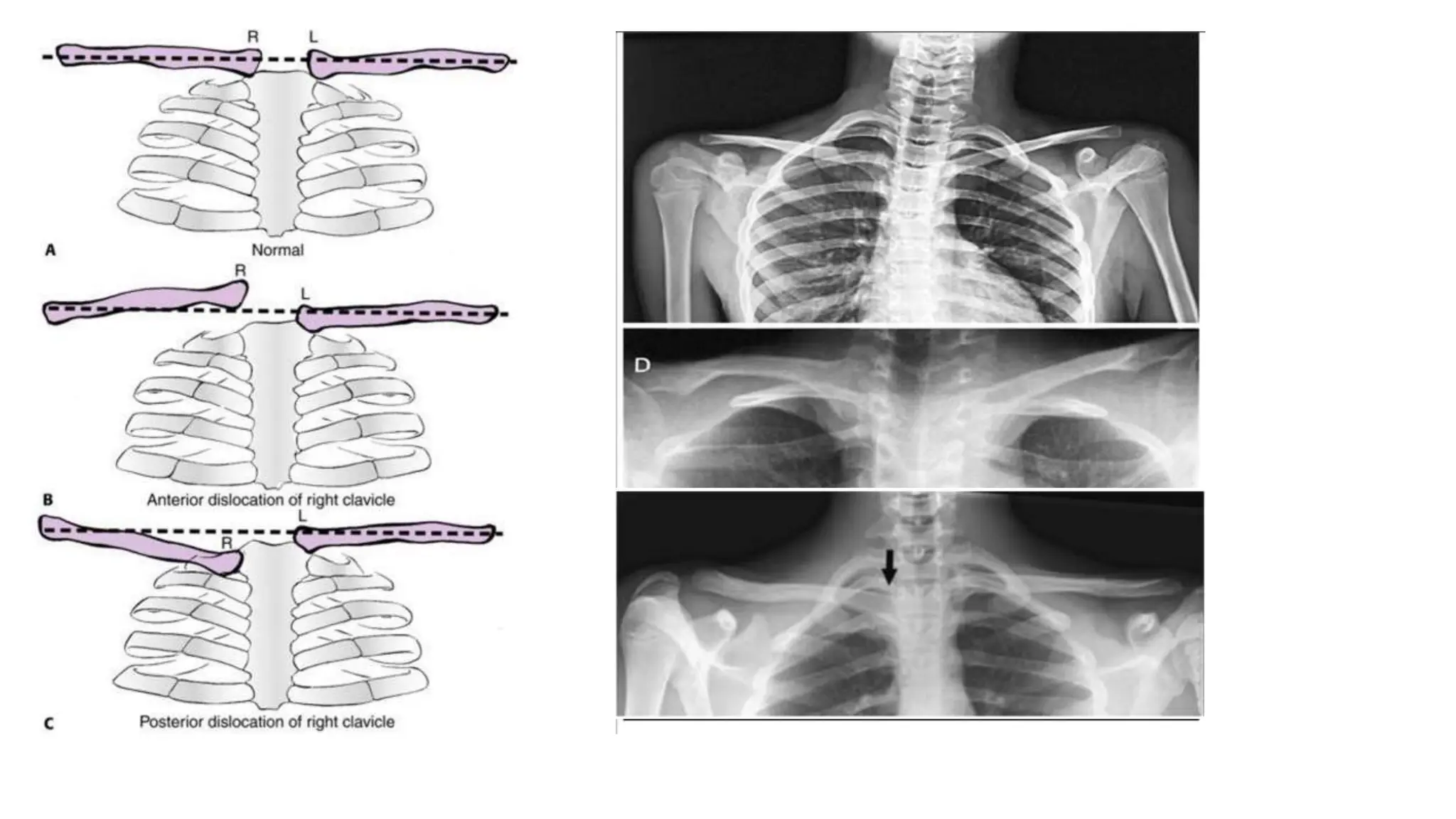
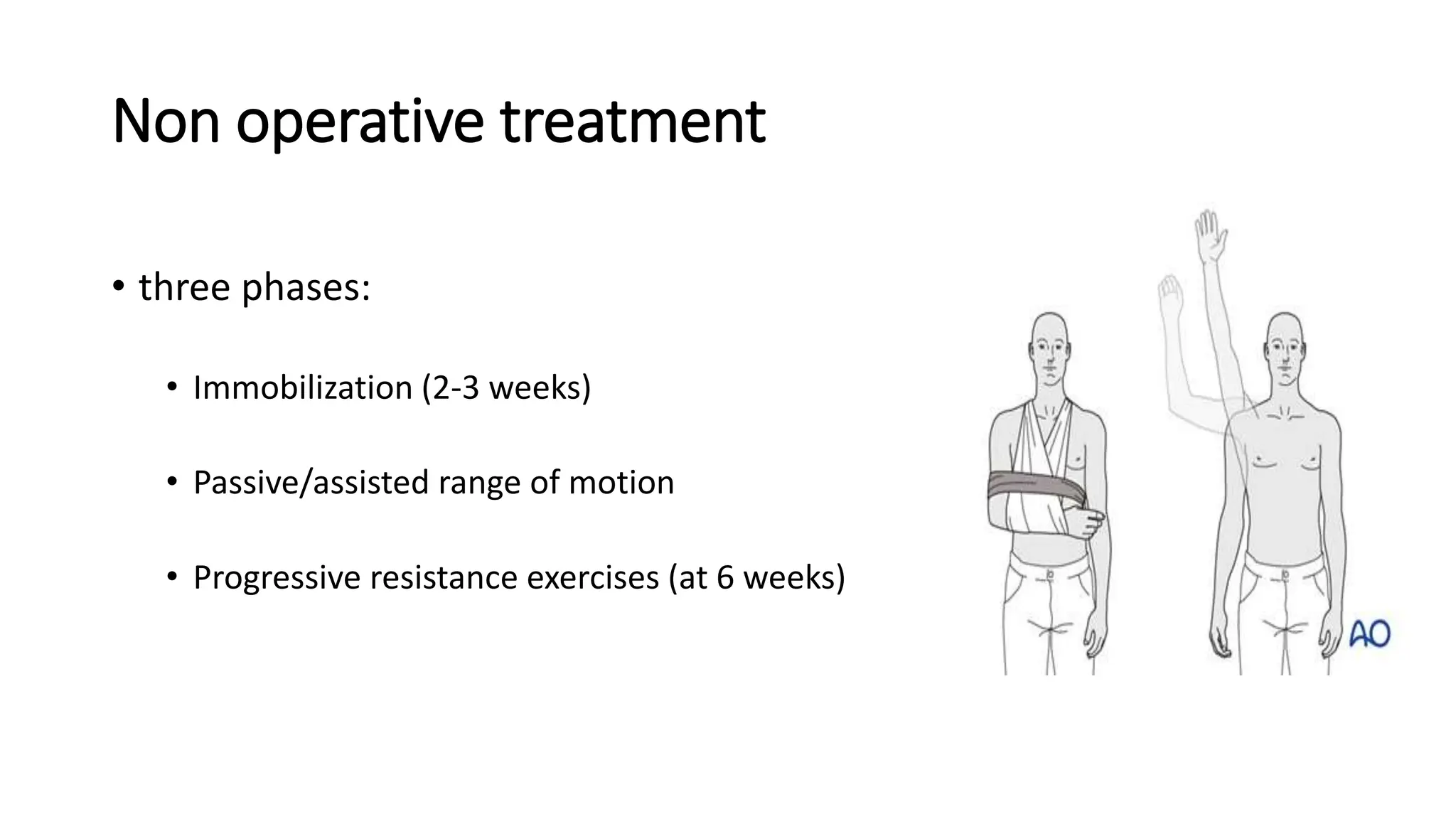
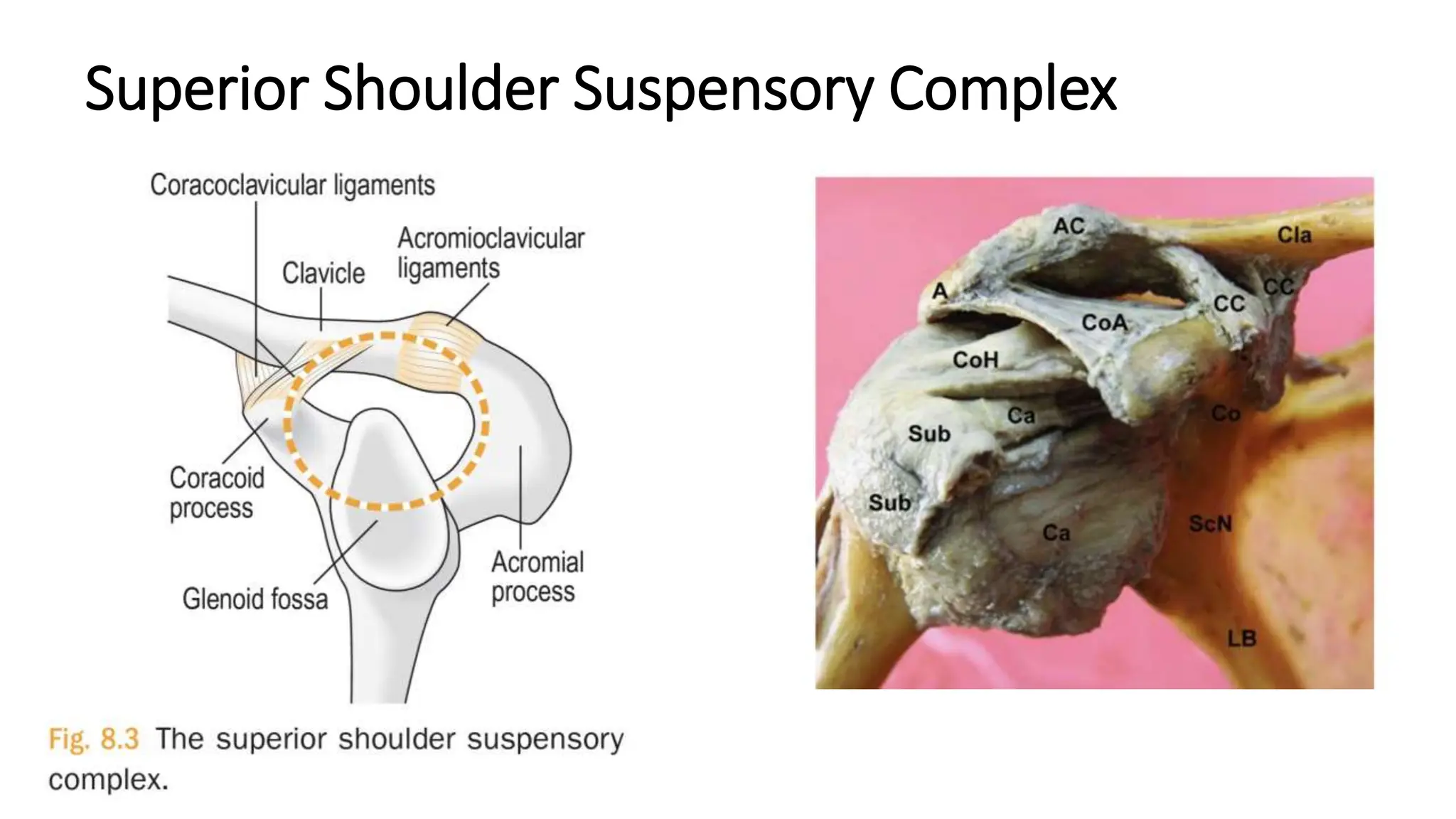
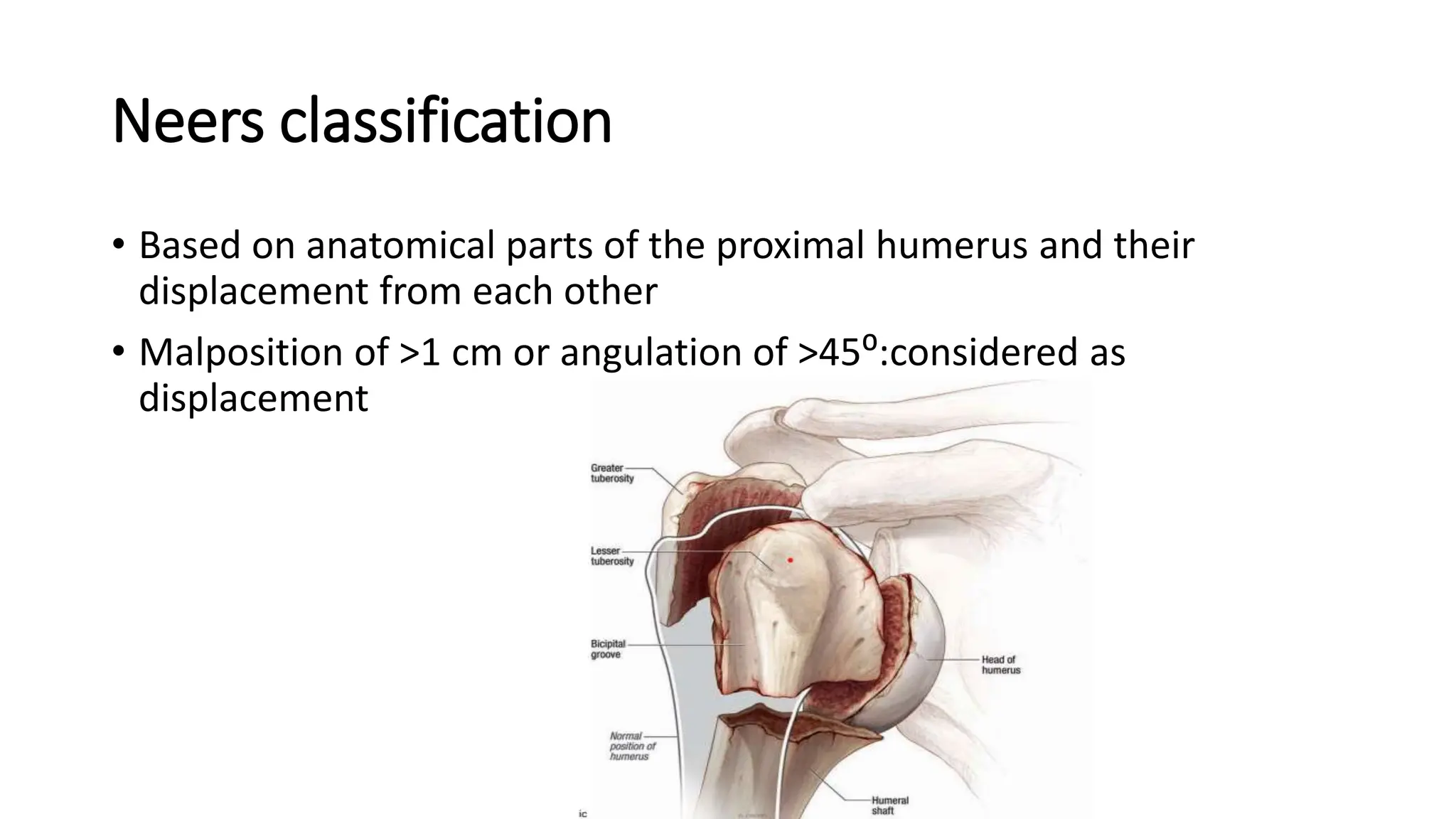
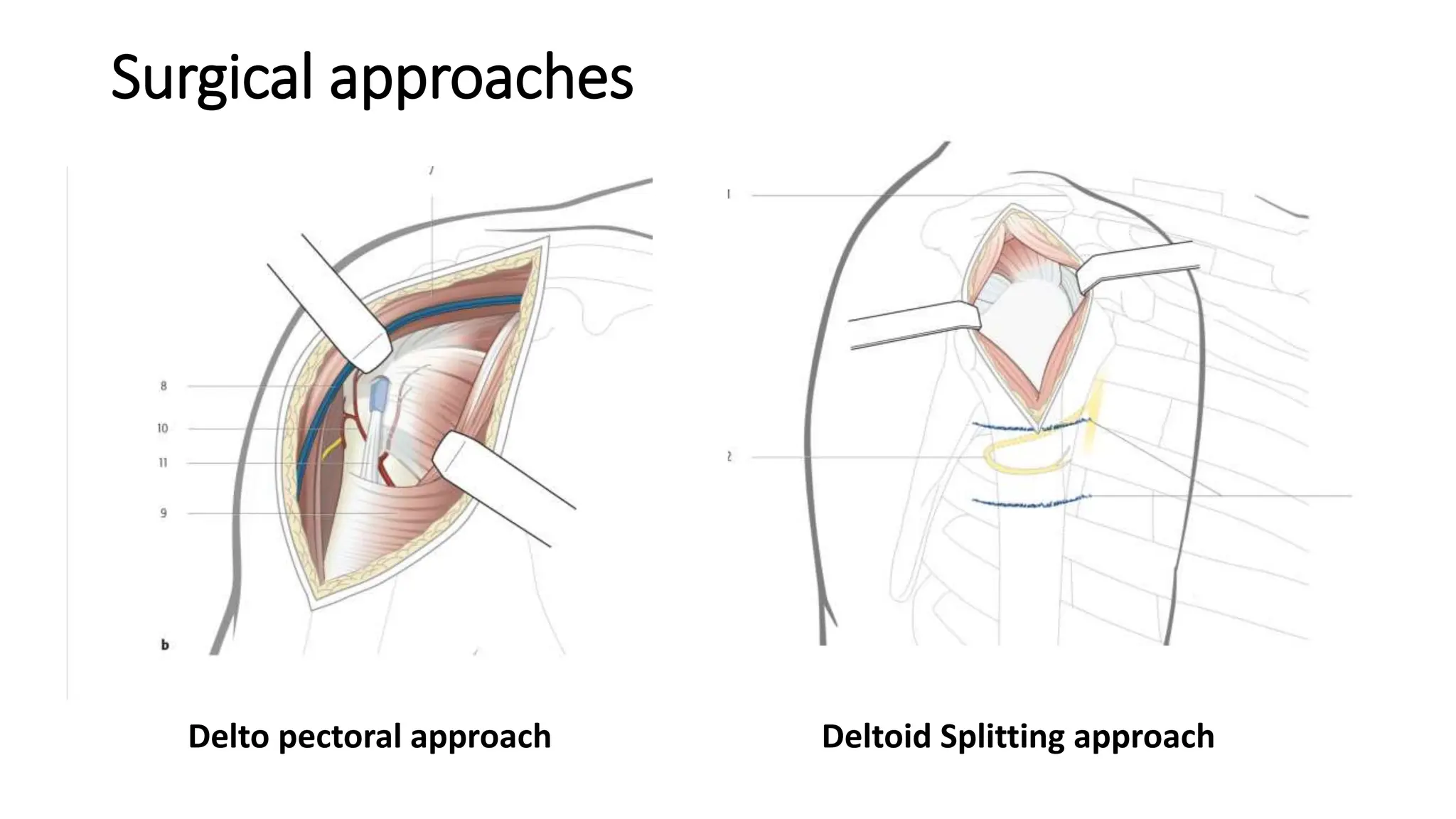
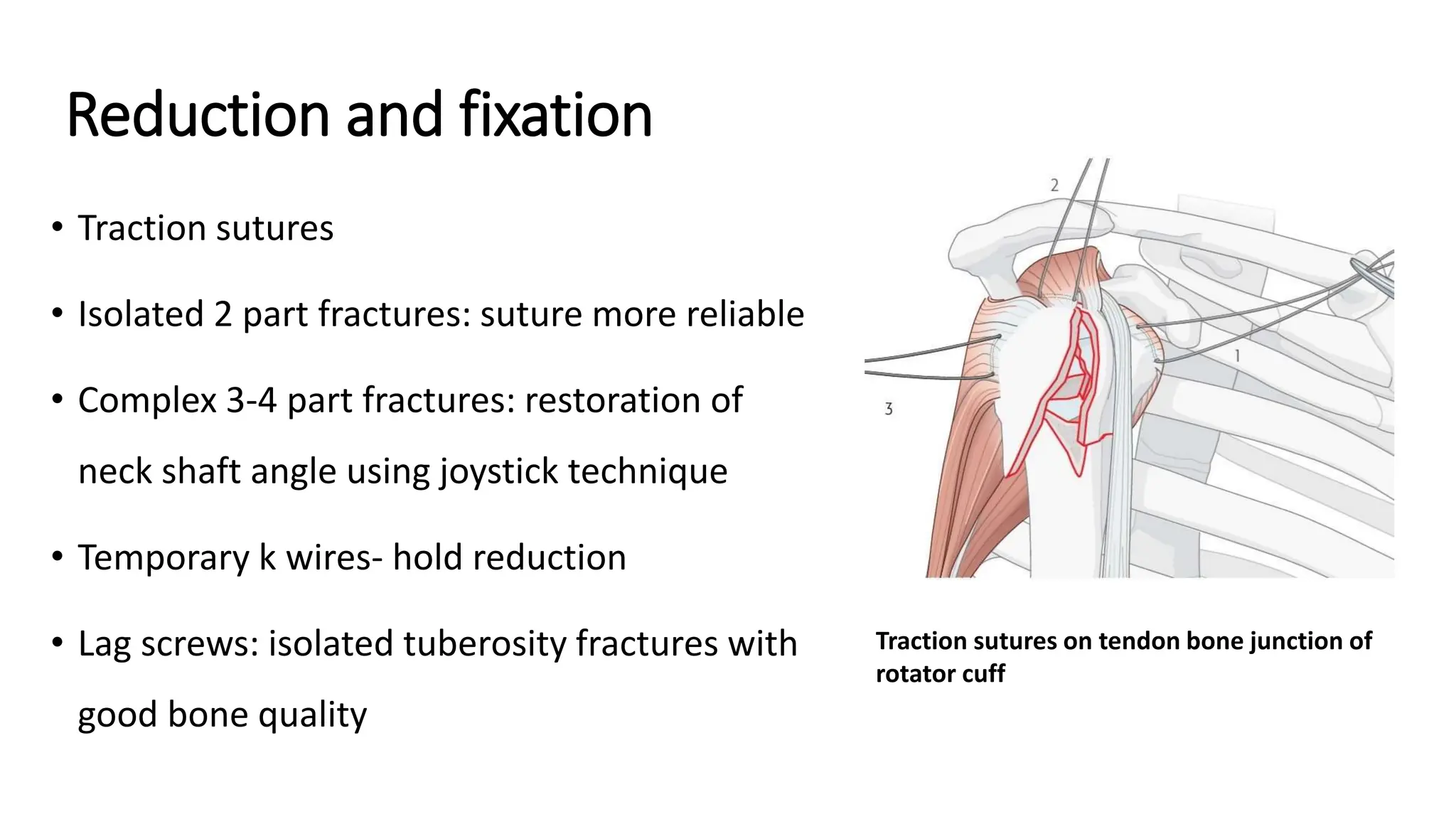
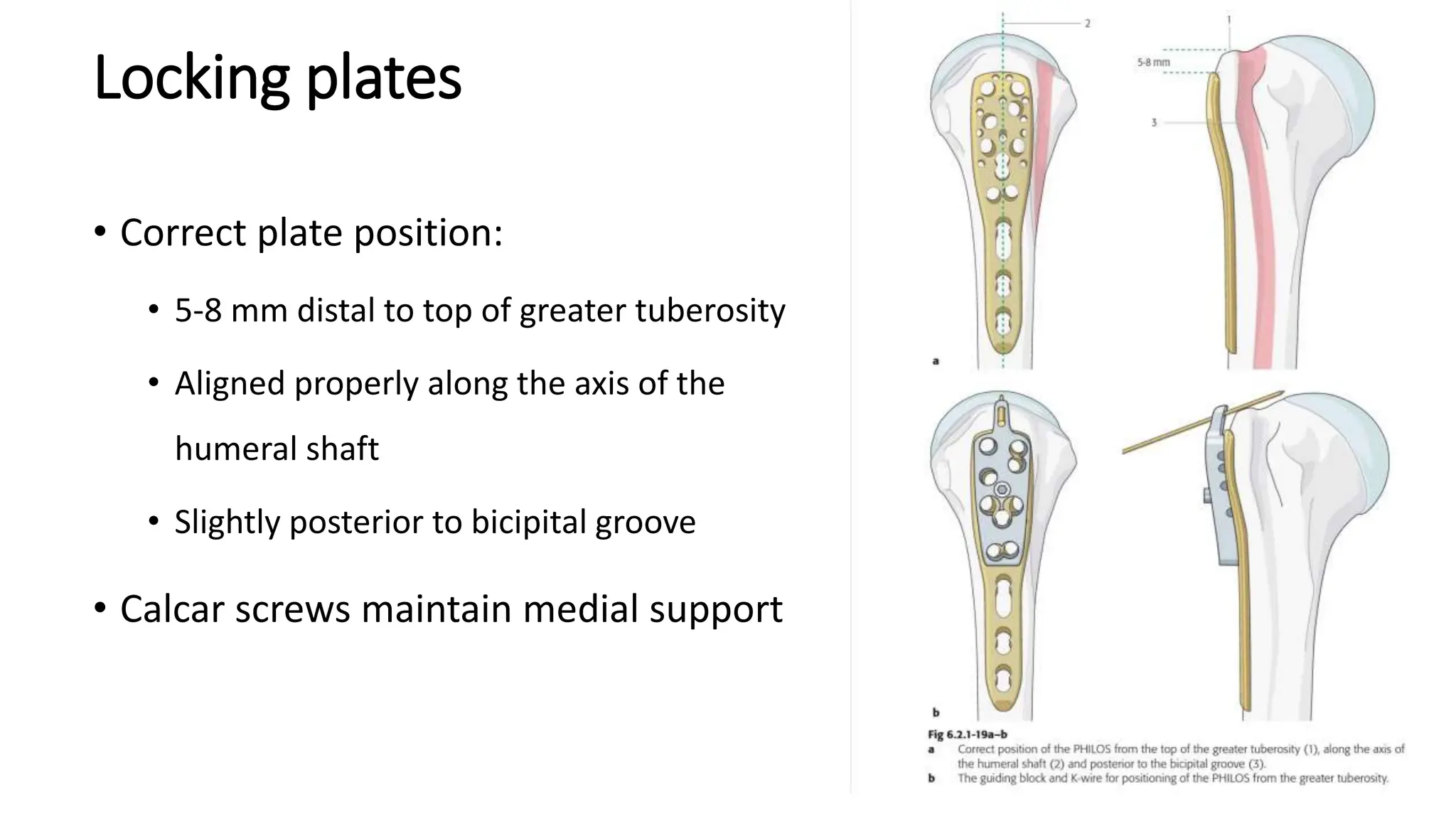
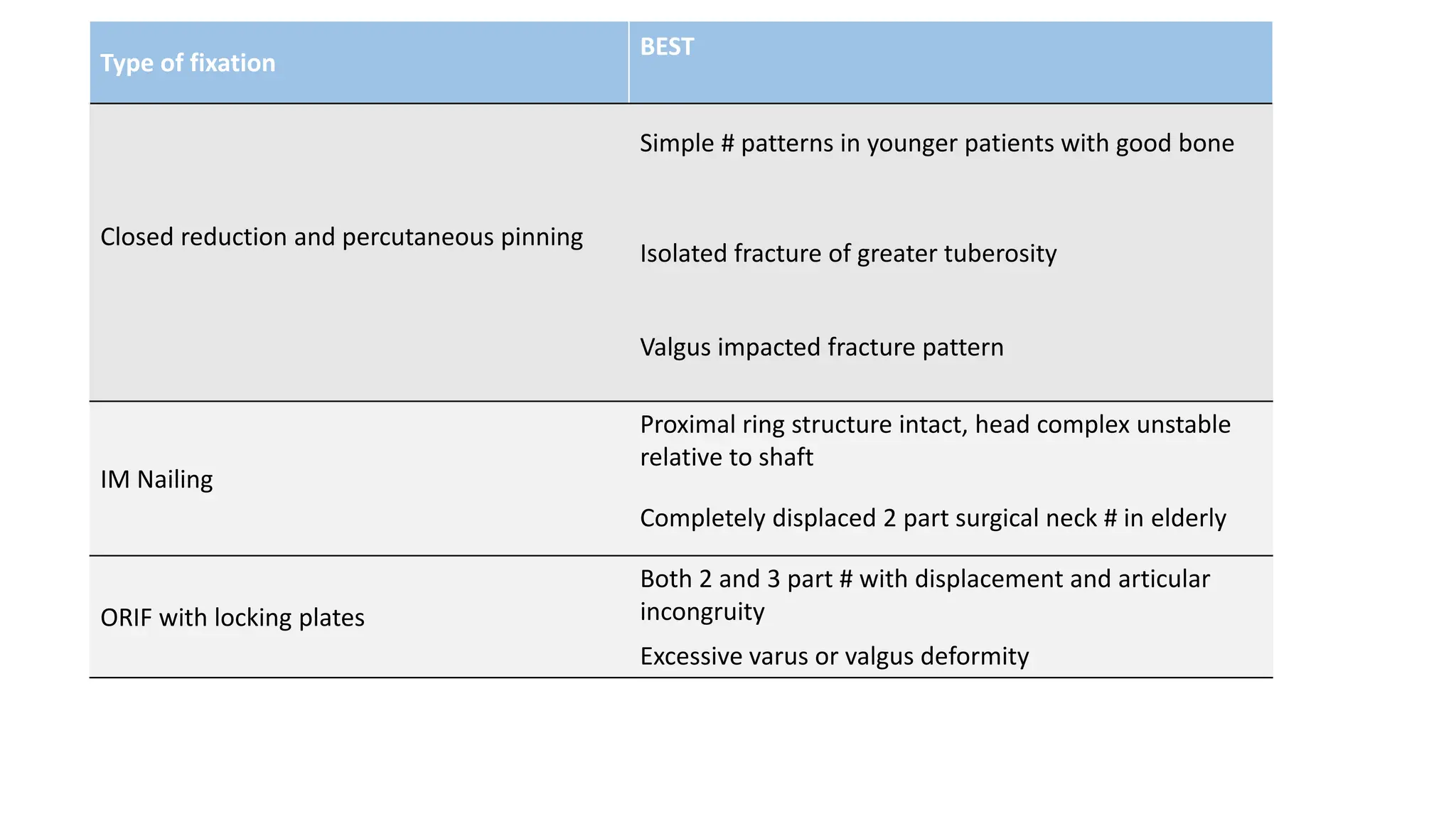
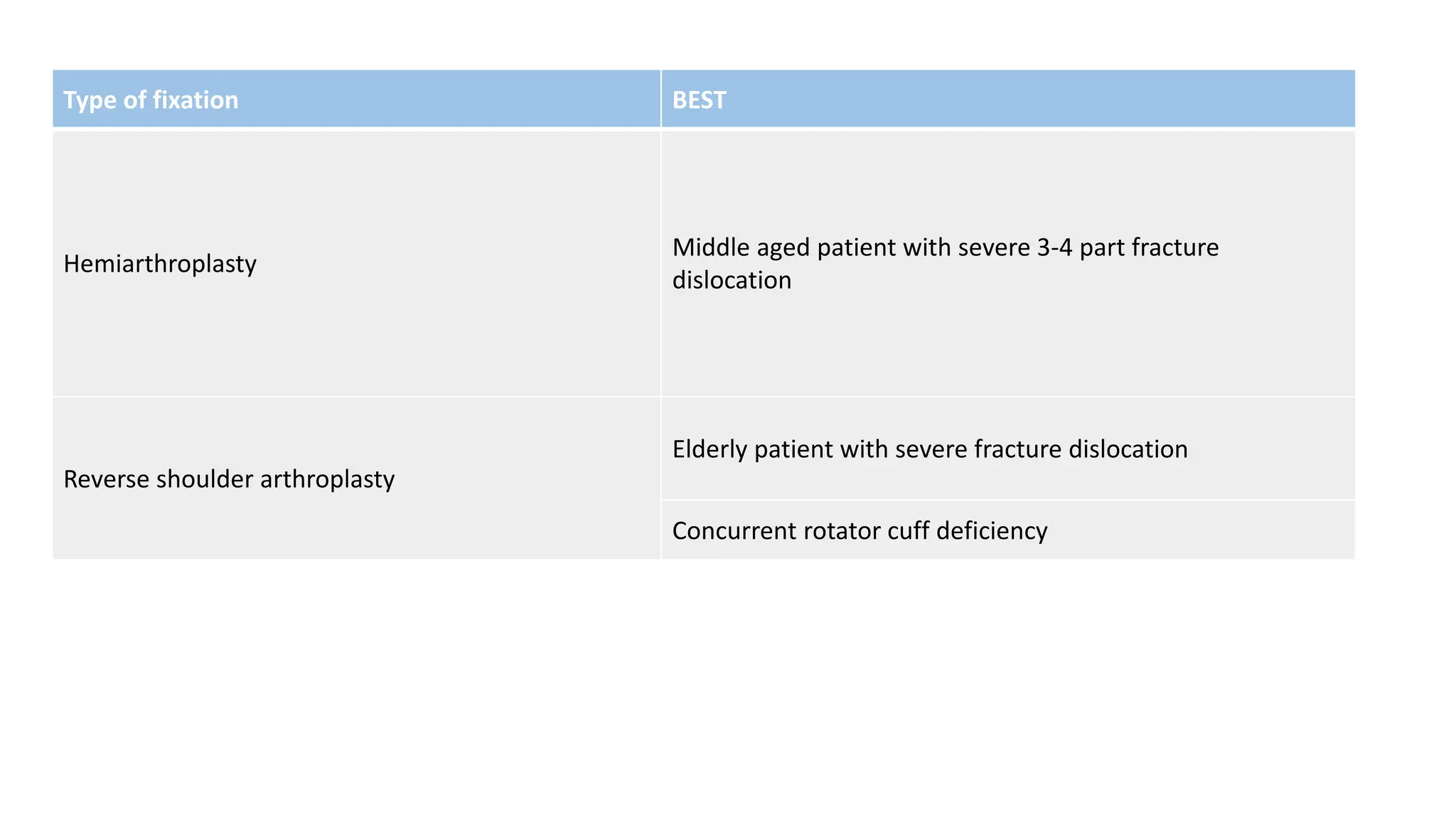
The document discusses various types of shoulder girdle fractures, including clavicle, scapula, and humerus fractures, and their classifications, clinical features, and management options. It details both non-operative and surgical treatments based on the type and severity of the fracture, highlighting complications and the importance of a thorough neurovascular assessment. Additionally, it emphasizes the relationship between shoulder girdle injuries and potential serious cardiothoracic and vascular injuries.