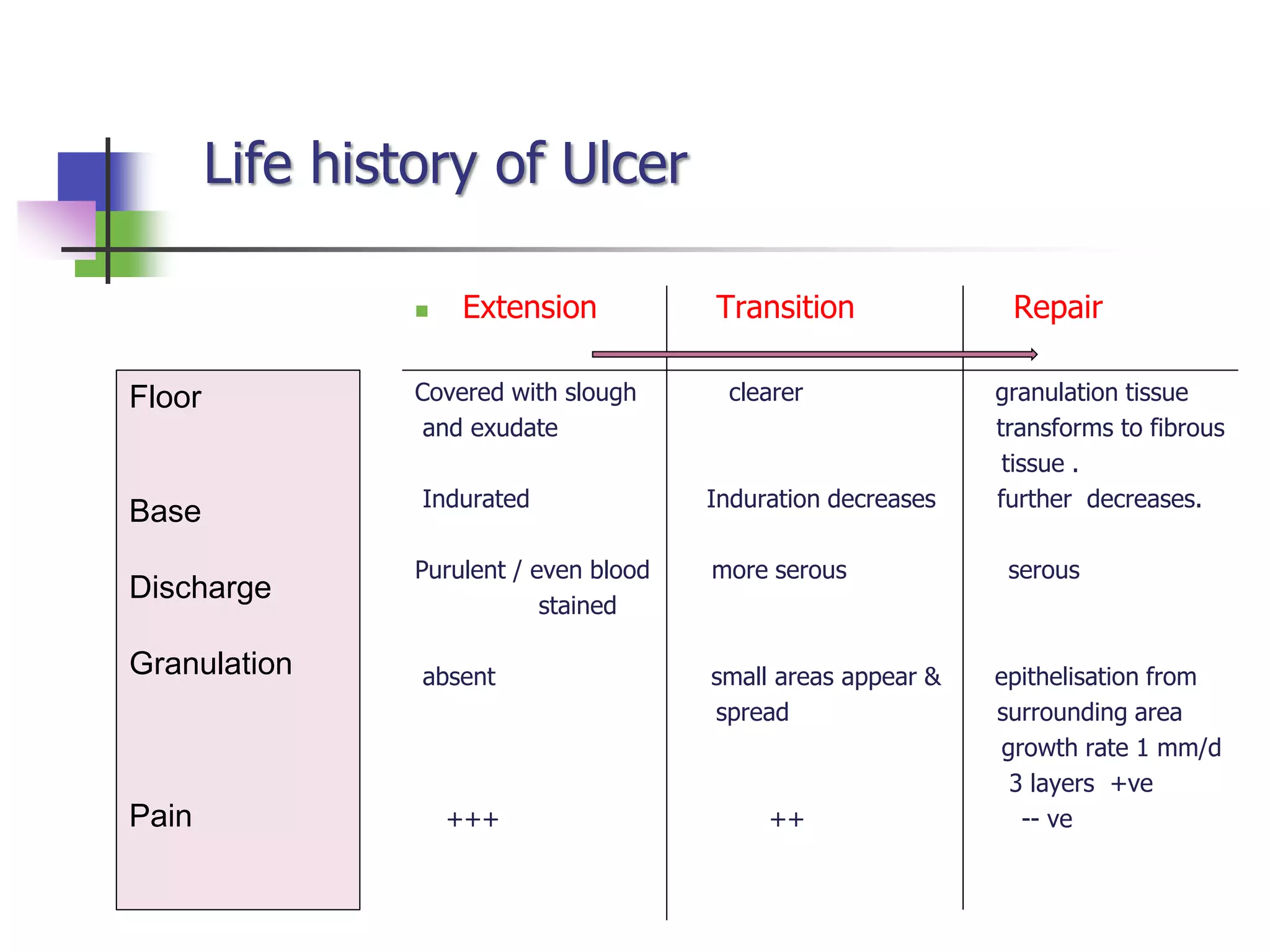
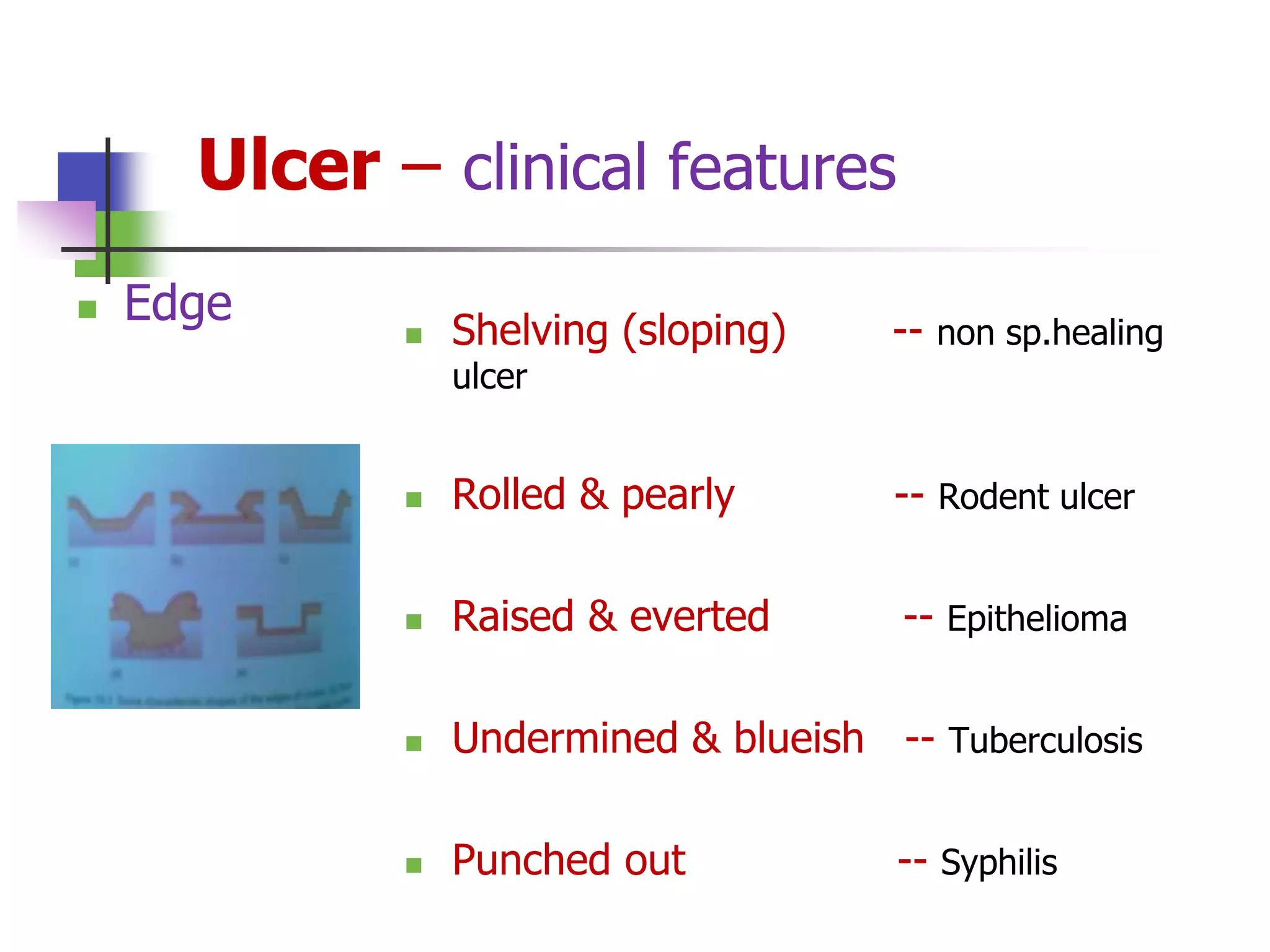
This document provides an overview of ulcers, including their classification, clinical features, investigations, and management principles. Ulcers are classified based on duration (acute vs chronic), etiology (infectious, physical/chemical agents, circulatory impairment), and location (Wagner's classification for foot ulcers). Clinical features include characteristics of the site, size, shape, edges, floor, base, discharge, pain levels, and surrounding lymph nodes. Investigations may include hematological and biochemical tests, imaging, biopsies, and microbiological cultures. Management principles focus on determining the underlying cause, correcting comorbidities, adequate drainage and debridement, treating any infection, and using appropriate dressings to promote healing.