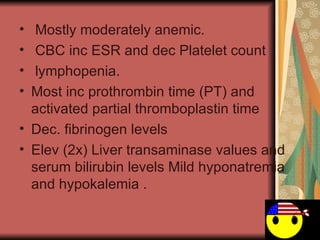
1. Enteric fever is a systemic infection caused by Salmonella typhi or paratyphi that results in a severe multisystem illness characterized by prolonged fever and bacterial invasion of organs.
2. S. typhi typically infects humans through contaminated food or water and spreads from the intestines to the bloodstream and organs like the liver, spleen and lymph nodes.
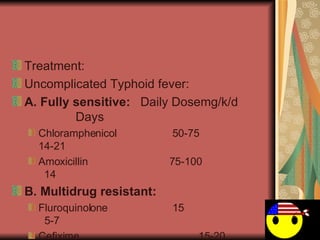
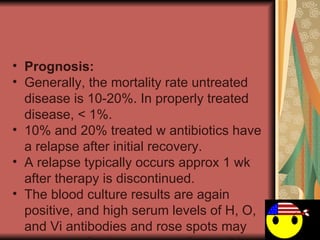
3. Treatment depends on antibiotic susceptibility but usually involves fluoroquinolones, third generation cephalosporins, or azithromycin. Relapse can occur in 10-20% of cases.