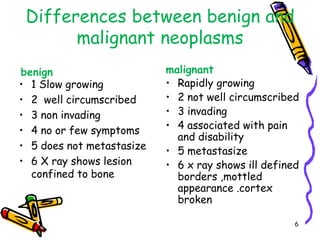
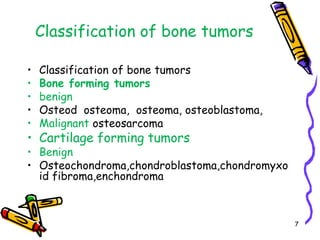
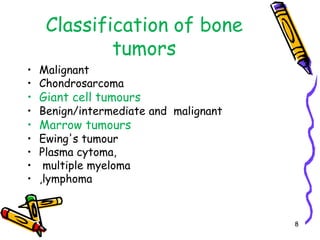
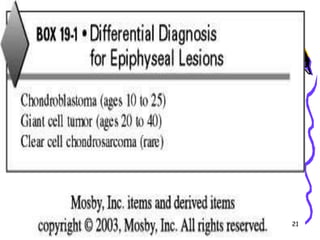
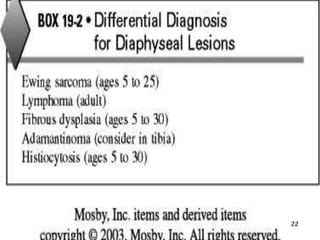
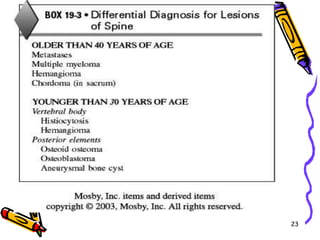
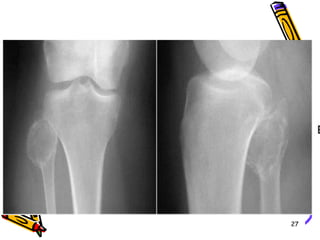
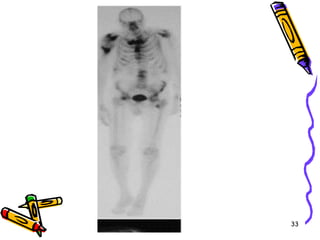
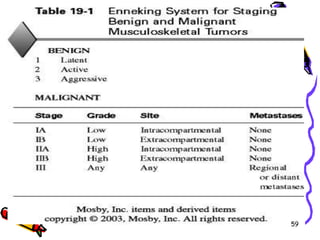
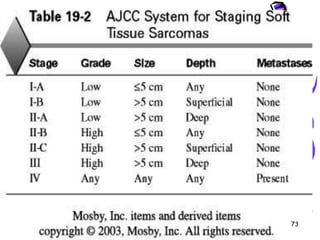
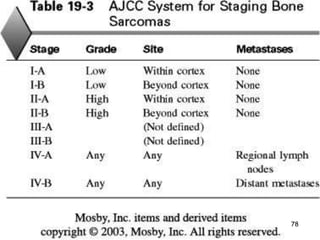
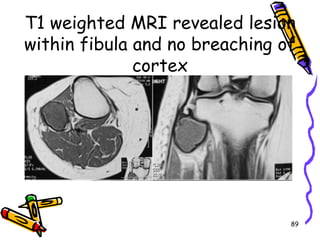
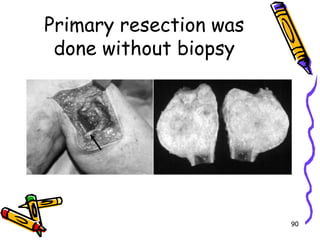
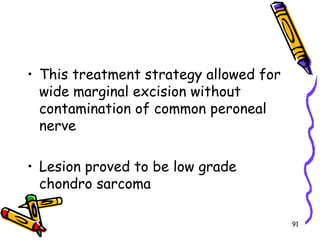
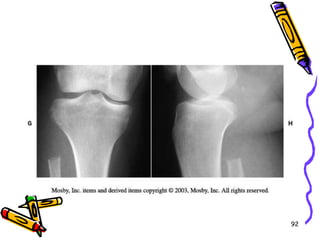
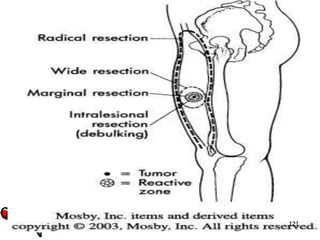
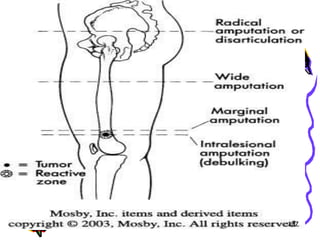
This document provides an overview of approaches to musculoskeletal neoplasms (tumors). It discusses the classification and staging of bone tumors, the evaluation and workup of patients, and treatment approaches including biopsy, surgery, radiation therapy, and chemotherapy. Specifically, it summarizes a case of a 51-year-old woman who presented with knee pain and was found to have a low-grade chondrosarcoma in her fibula that was successfully treated with wide excision without preoperative biopsy.