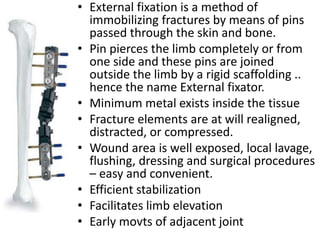
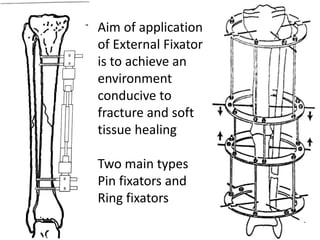
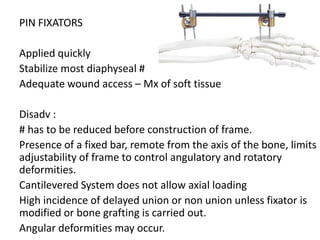
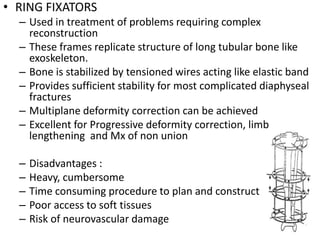
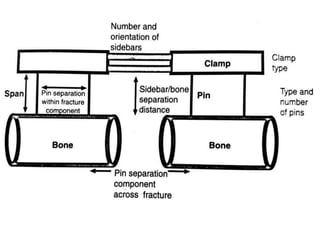
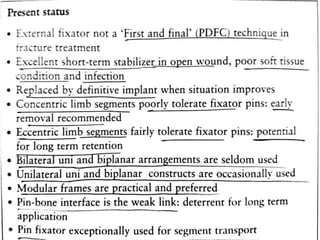
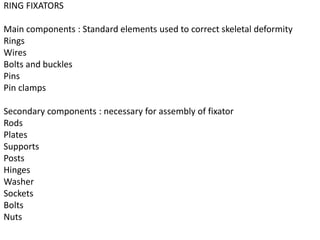
External fixators are used to immobilize fractures by inserting pins through the skin and bone that are connected by a rigid scaffolding outside the limb. There are two main types - pin fixators and ring fixators. Pin fixators are applied quickly but have limitations in controlling deformities, while ring fixators can achieve complex reconstruction but are heavier. Professor Gavril Ilizarov developed ring fixators in the 1950s which use tensioned wires between rings to stabilize fractures. Ring fixators can be used to treat limb lengthening, deformity correction, non-unions, joint contractures and more complex fractures. They work by gradually distracting the bone between rings.