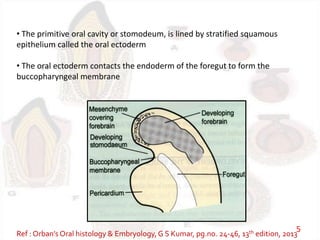
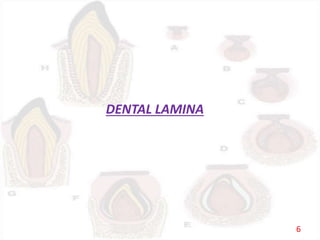
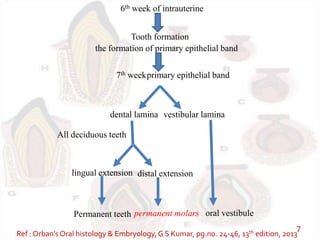
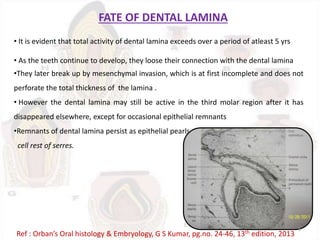
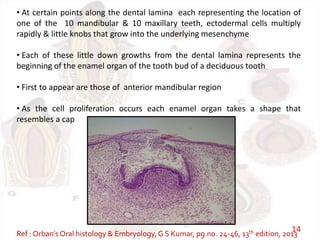
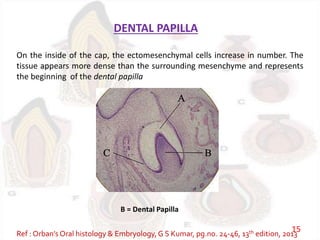
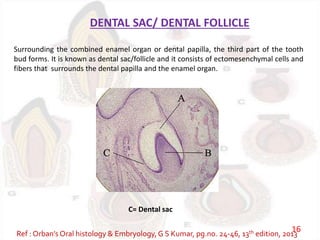
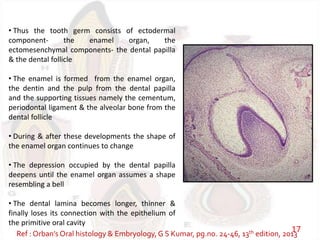
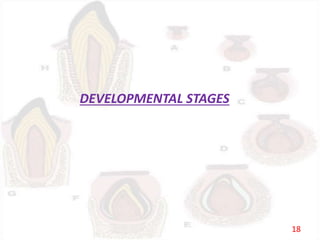
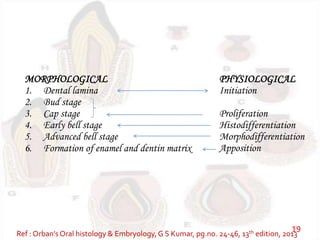
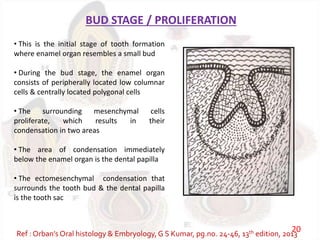
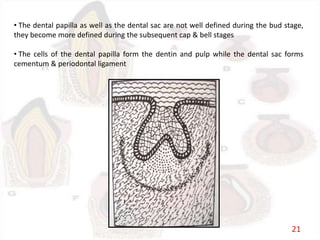
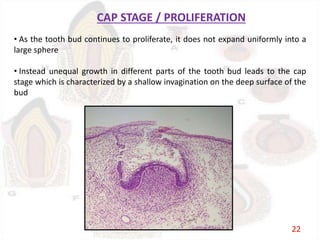
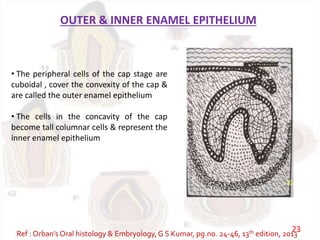
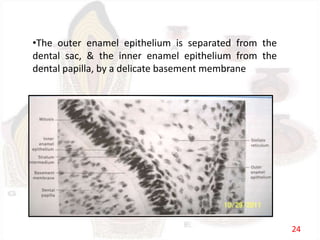
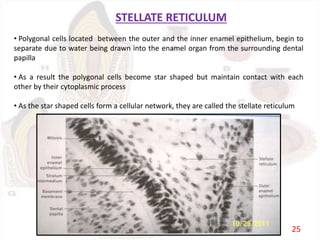
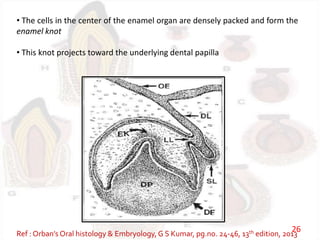
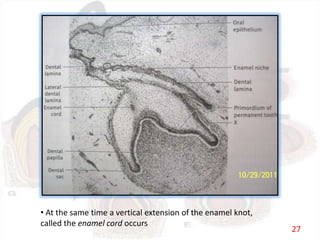
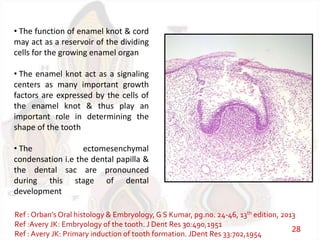
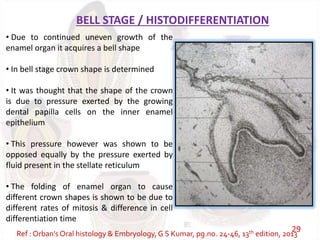
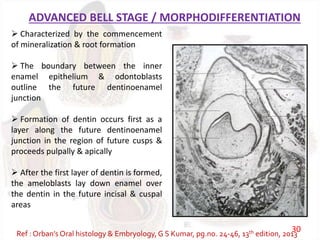
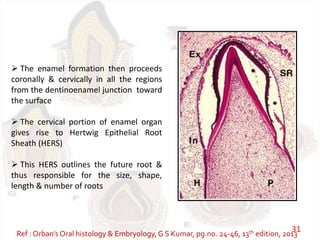
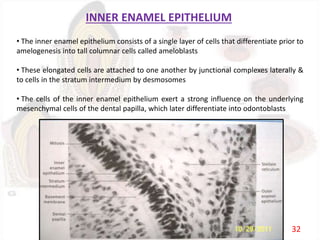
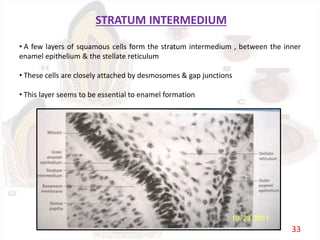
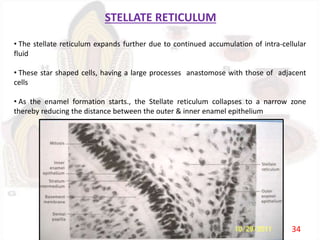
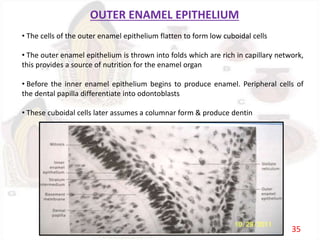
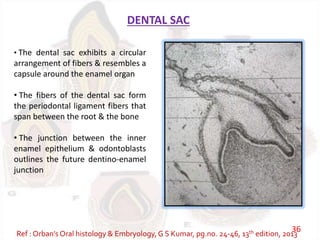
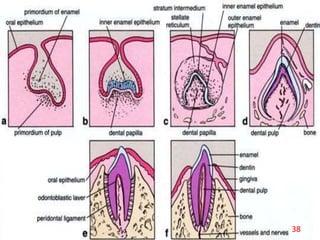
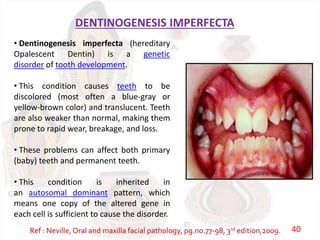
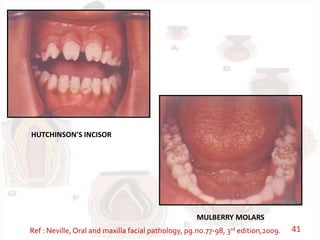
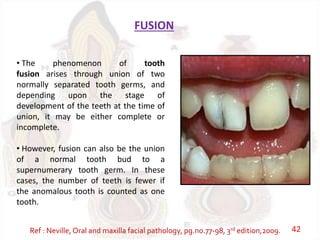
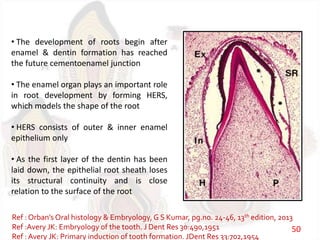
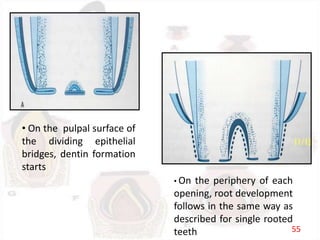
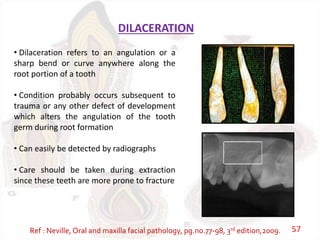
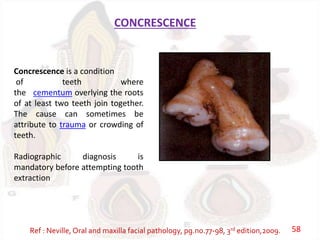
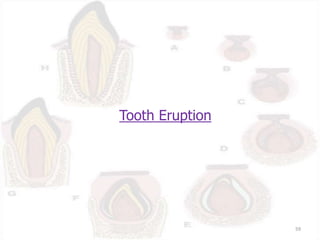
The document discusses the development of teeth from the dental lamina stage through the various bell stages. It describes how the enamel organ, dental papilla, and dental sac form and their roles in tooth development. The stages of tooth development including bud, cap, and bell stages are summarized. Clinical conditions related to abnormalities in tooth development like dentinogenesis imperfecta, Hutchinson's incisor, and fusion are also mentioned.