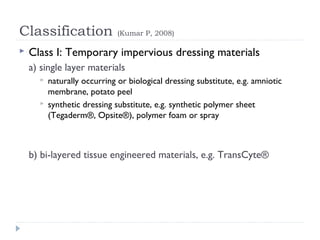
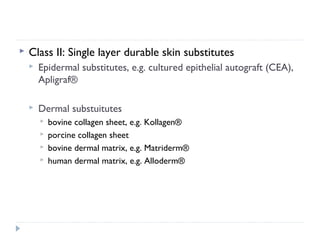
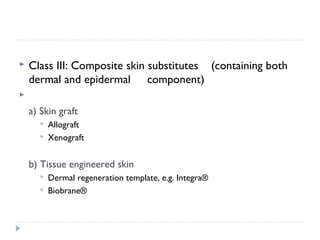
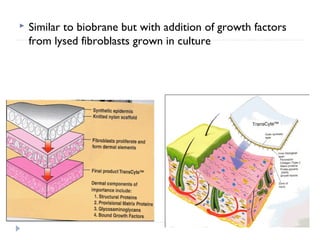
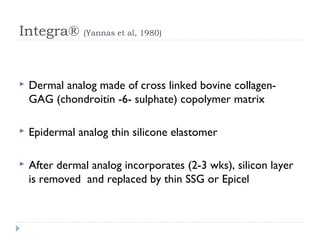
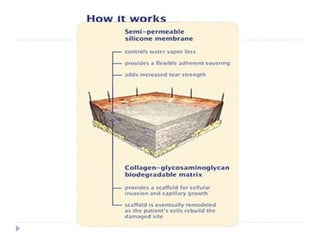
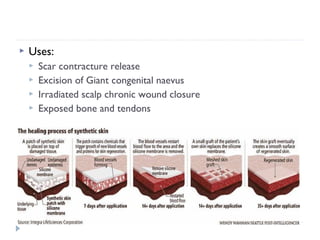
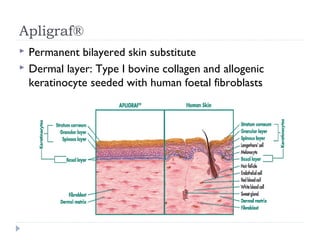
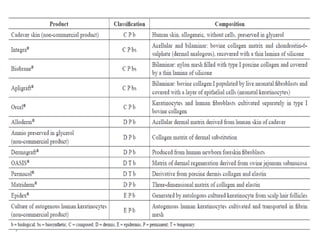
This document discusses skin substitutes, which are materials that can aid in wound closure and replace skin functions temporarily or permanently. It defines various types of skin substitutes and outlines their classification. It describes both temporary skin substitutes like porcine xenografts, human allografts, and synthetic options. It also discusses permanent skin substitutes that contain dermal and epidermal components, such as Integra, Apligraf, and cultured epithelial autografts. The document concludes that skin substitutes are important in plastic surgery and wound management but are limited by high costs and availability.