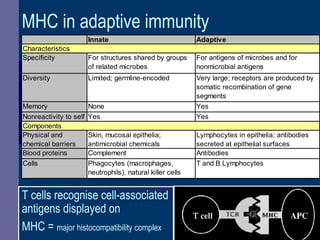
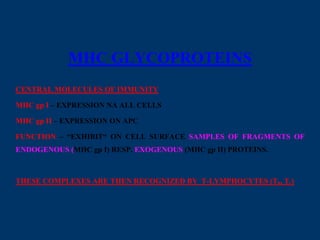
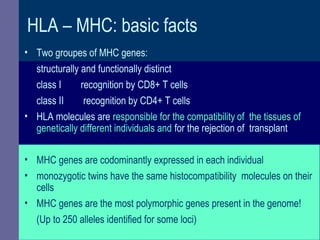
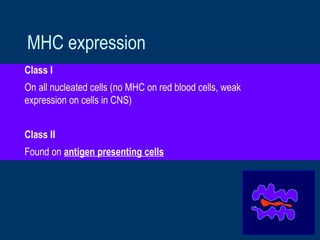
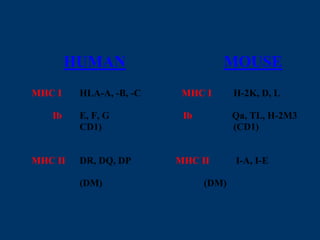
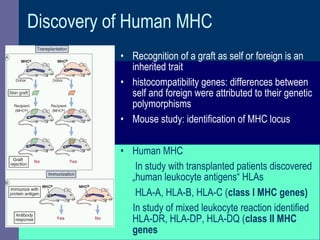
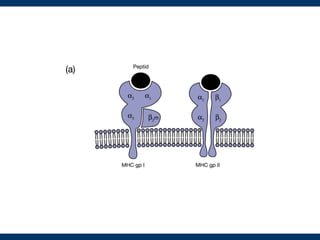
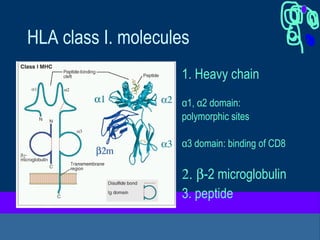
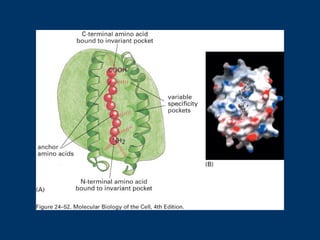
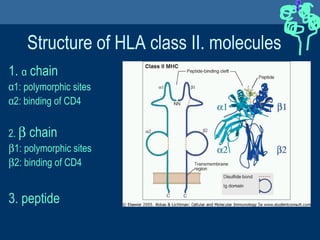
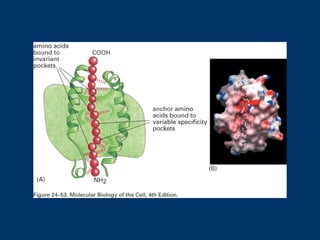
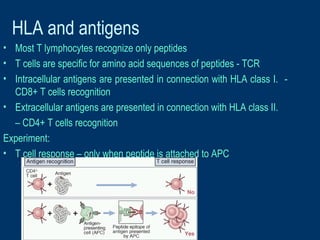
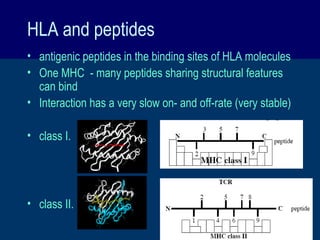
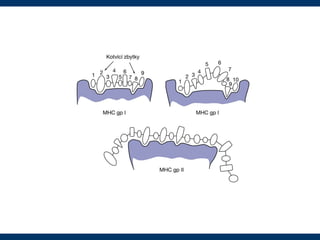
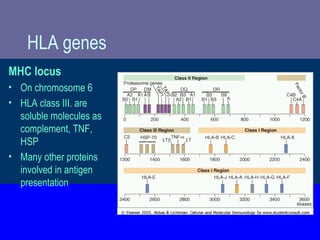
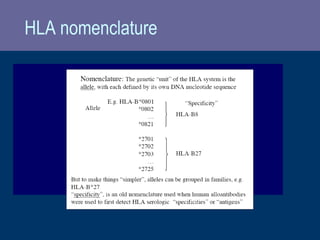
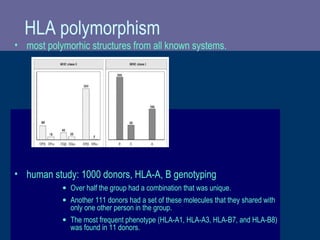
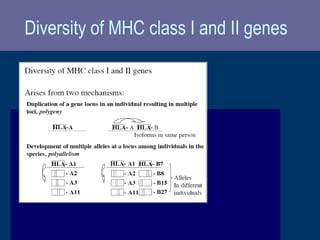
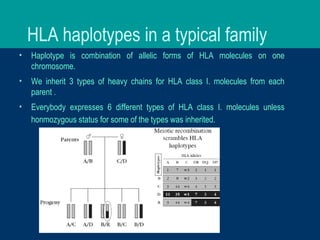
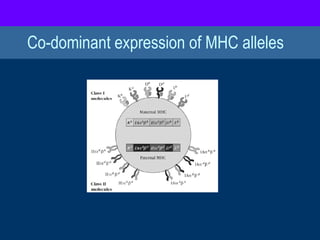
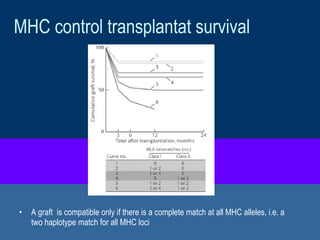
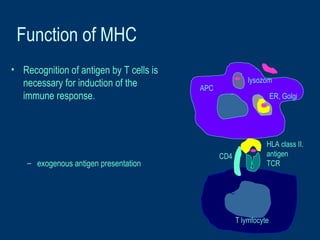
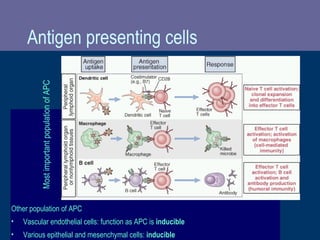
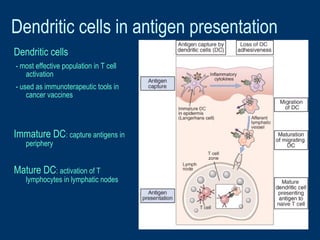
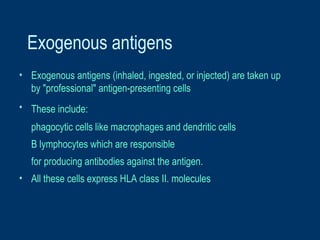
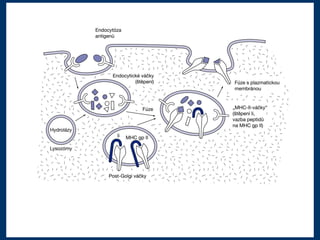
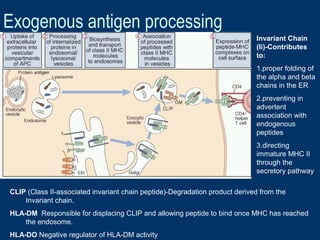
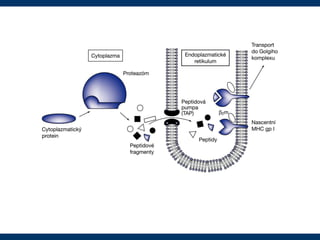
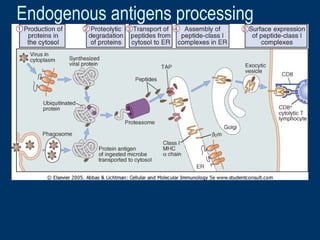
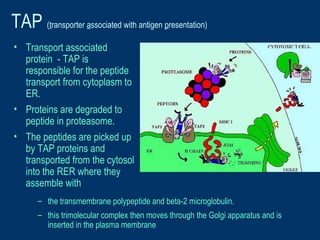
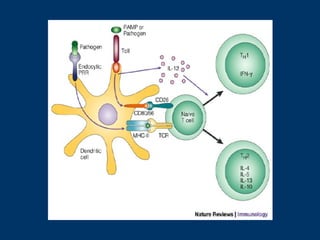
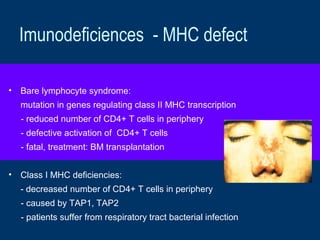
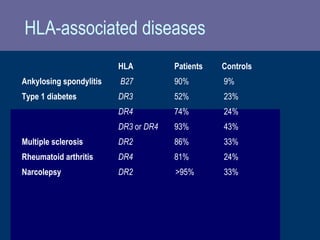
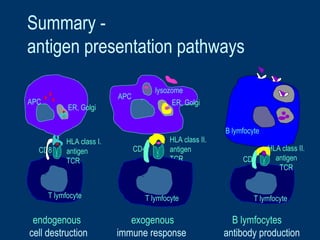
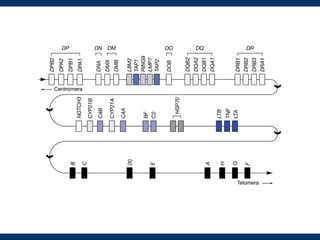
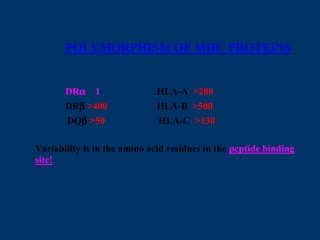
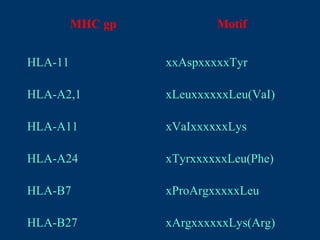
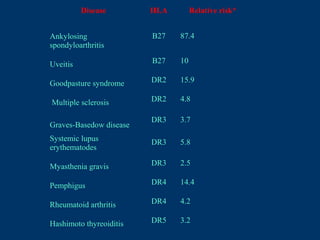
The document provides an overview of the major histocompatibility complex (MHC), specifically human leukocyte antigens (HLA), and their role in adaptive immunity. It discusses the structure and function of different classes of MHC molecules, their genetic polymorphism, and the significance of antigen presentation in immune responses. The document also highlights associations between HLA types and various diseases, along with the importance of antigen-presenting cells in T cell activation.