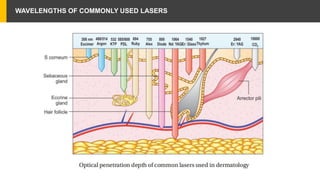
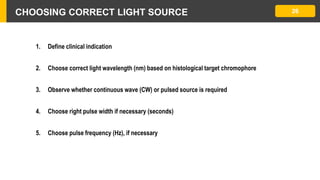
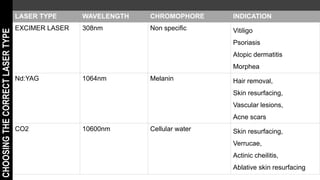
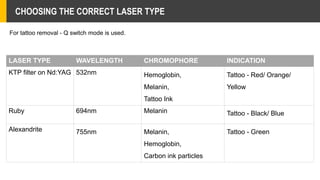
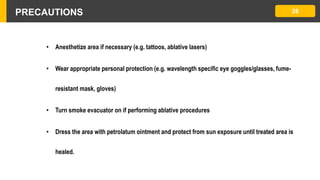
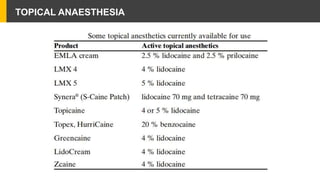
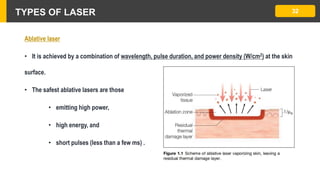
This document provides an overview of laser therapy basics. It discusses the principles of lasers, including how they work by stimulating emission of radiation. It describes the different types of lasers categorized by their lasing medium (solid, gas, liquid) and wavelengths commonly used (CO2, Nd:YAG, excimer). The document explains principles of selective photothermolysis and how parameters like wavelength, pulse duration, and skin cooling can be optimized for specific clinical indications and target chromophores in the skin.