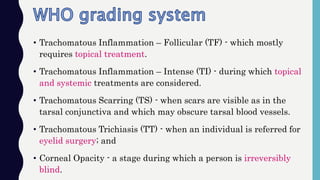
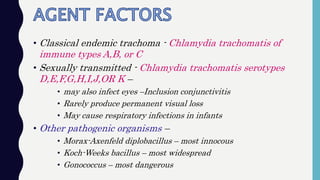
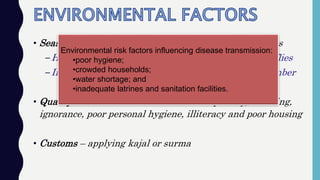
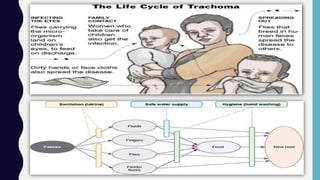
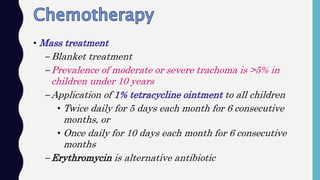
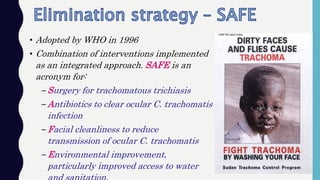
Trachoma is a chronic infectious disease of the conjunctiva and cornea caused by the bacterium Chlamydia trachomatis. It progresses through inflammatory stages and can cause scarring of the conjunctiva and eyelids leading to entropion, trichiasis, and corneal opacity resulting in blindness. Trachoma was a major public health problem in India in the 1950s but intensive efforts through the National Trachoma Control Programme and WHO's SAFE strategy of surgery, antibiotics, facial cleanliness and environmental improvement have helped eliminate trachoma as a public health problem in India by 2017. Constant surveillance is still needed to prevent resurgence.