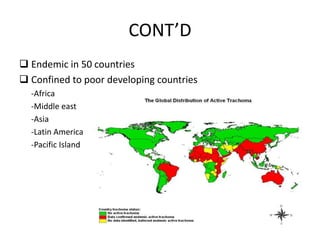
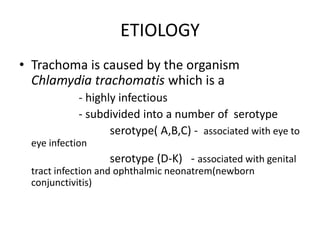
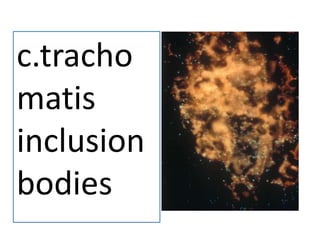
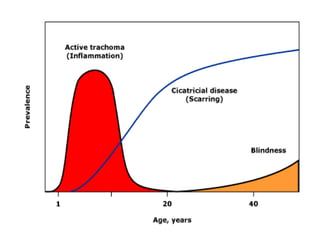
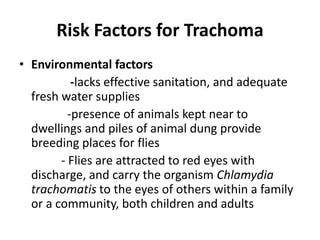
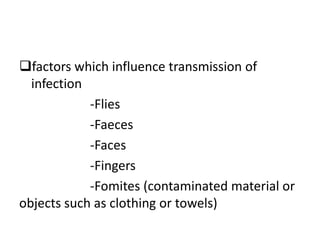
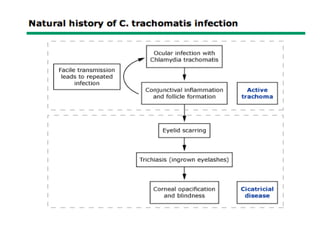
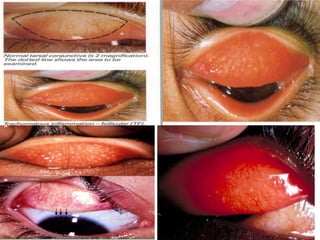
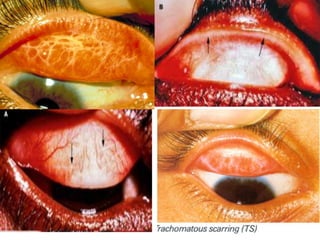
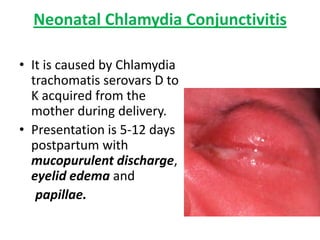
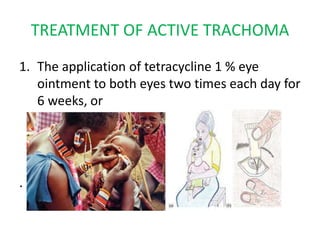
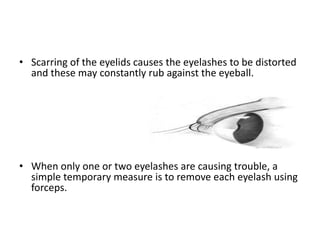
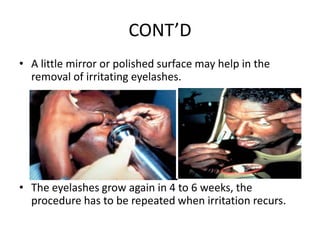
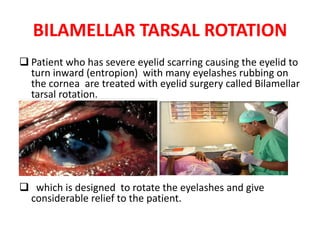
This document provides information about trachoma including its definition, epidemiology, etiology, risk factors, clinical presentation, diagnosis, treatment and prevention. Trachoma is caused by Chlamydia trachomatis and is the world's leading infectious cause of blindness. It is endemic in poor, rural areas with lack of water and sanitation. Clinical stages include active trachoma and scarring trachoma which can lead to trichiasis and corneal opacity. Treatment involves antibiotics and surgery. Prevention focuses on hygiene, sanitation and the SAFE strategy promoted by WHO to eliminate trachoma by 2020.