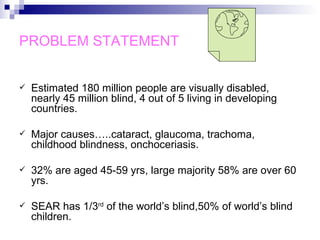
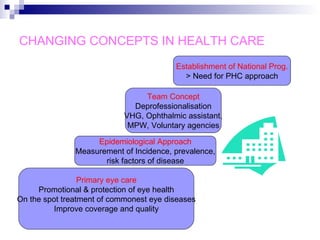
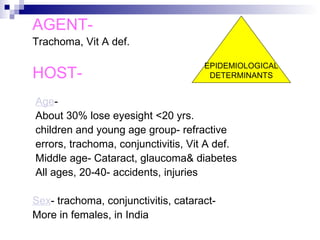
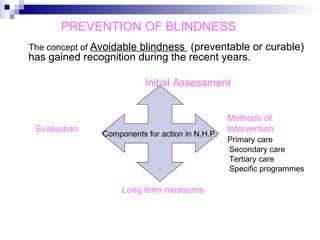
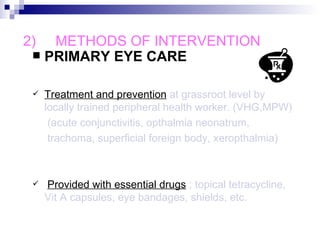
The document discusses blindness, including its definition, categories of visual impairment, major causes, and the problem statement. It covers changing concepts in healthcare with regards to eye care and prevention of blindness through primary, secondary and tertiary prevention methods. The Vision 2020 initiative to eliminate avoidable blindness is also summarized. Major causes of blindness in India are discussed, along with epidemiological determinants and methods of intervention through primary, secondary and tertiary care. Specific prevention programs like trachoma control, vitamin A prophylaxis and occupational eye health services are highlighted.