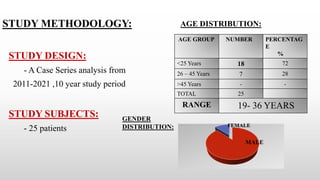
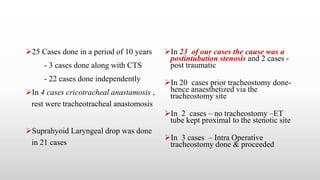
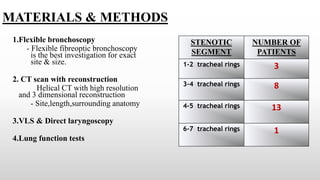
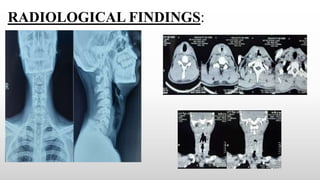
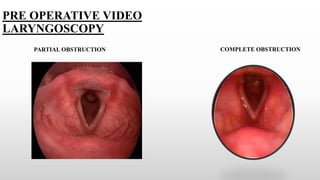
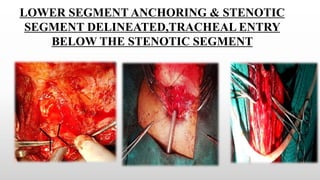
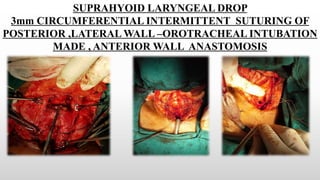
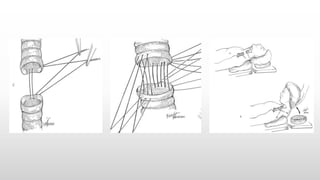
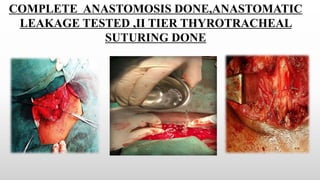
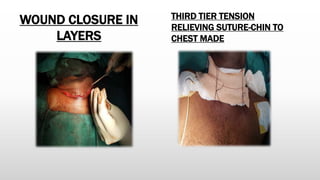
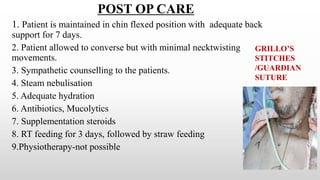
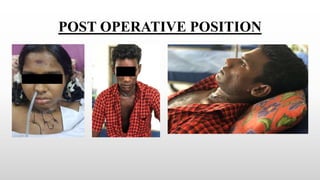
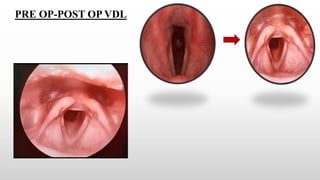
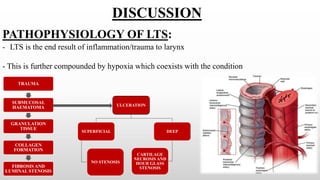
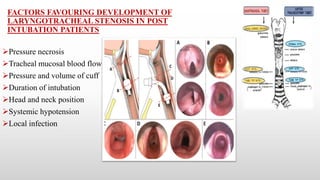
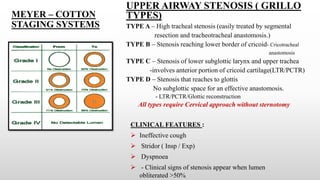
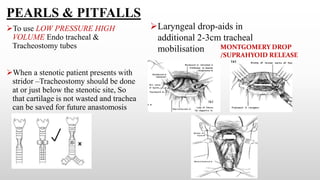
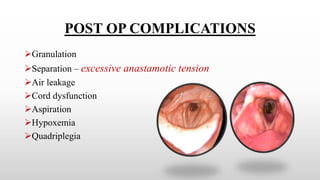
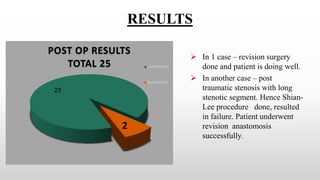
This case series analyzes 25 patients with tracheal stenosis treated between 2011-2021. Most patients were younger than 25 years old and the stenosis was caused by intubation in 23 cases. Surgical techniques included tracheal resection and anastomosis. Outcomes were successful in 23 cases, with only 2 cases experiencing restenosis. The conclusion emphasizes that tracheal resection and reconstruction can successfully treat stenosis when performed by experienced surgeons, with careful attention to anatomy and tension-relieving sutures for wound healing.