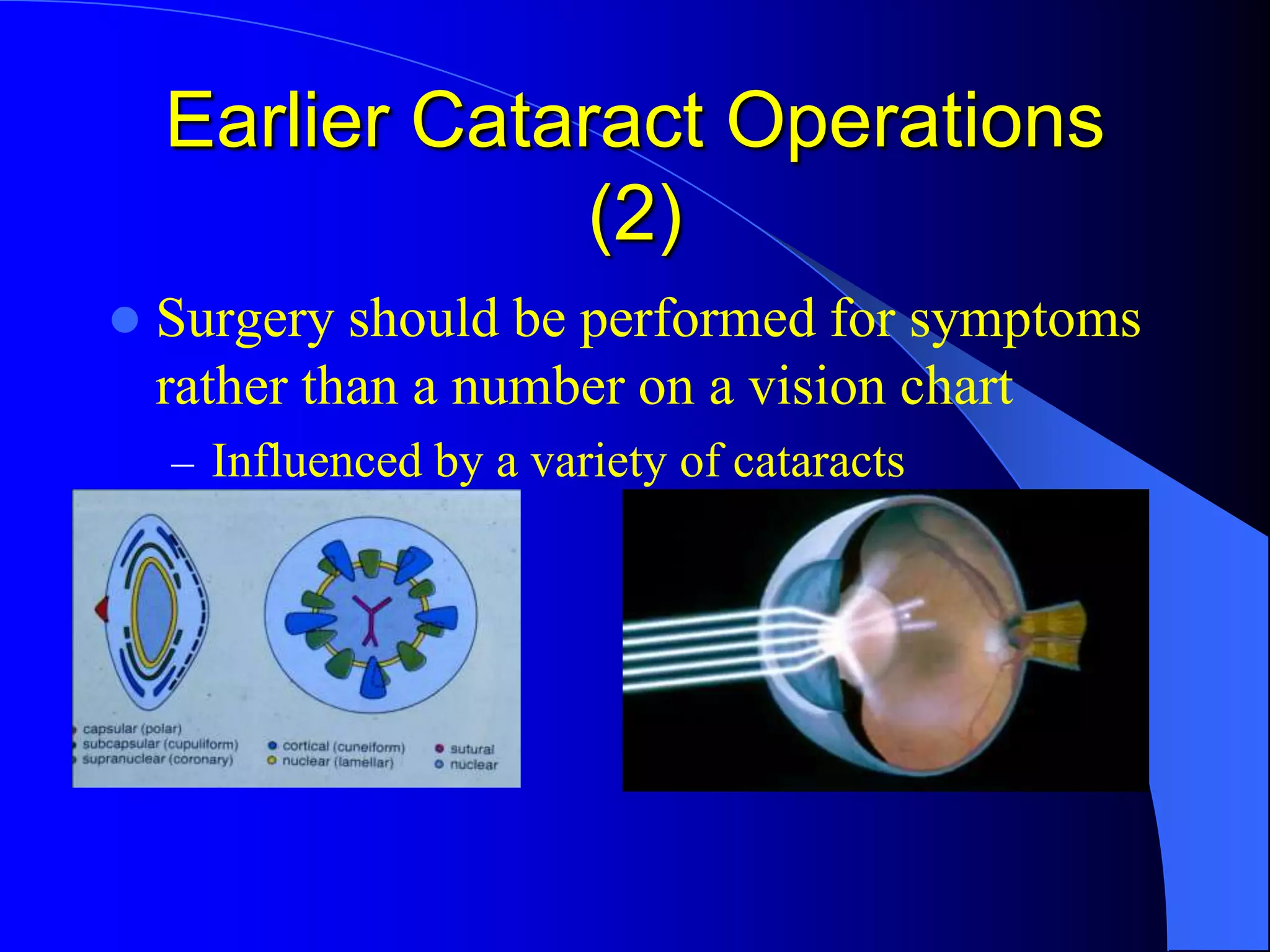
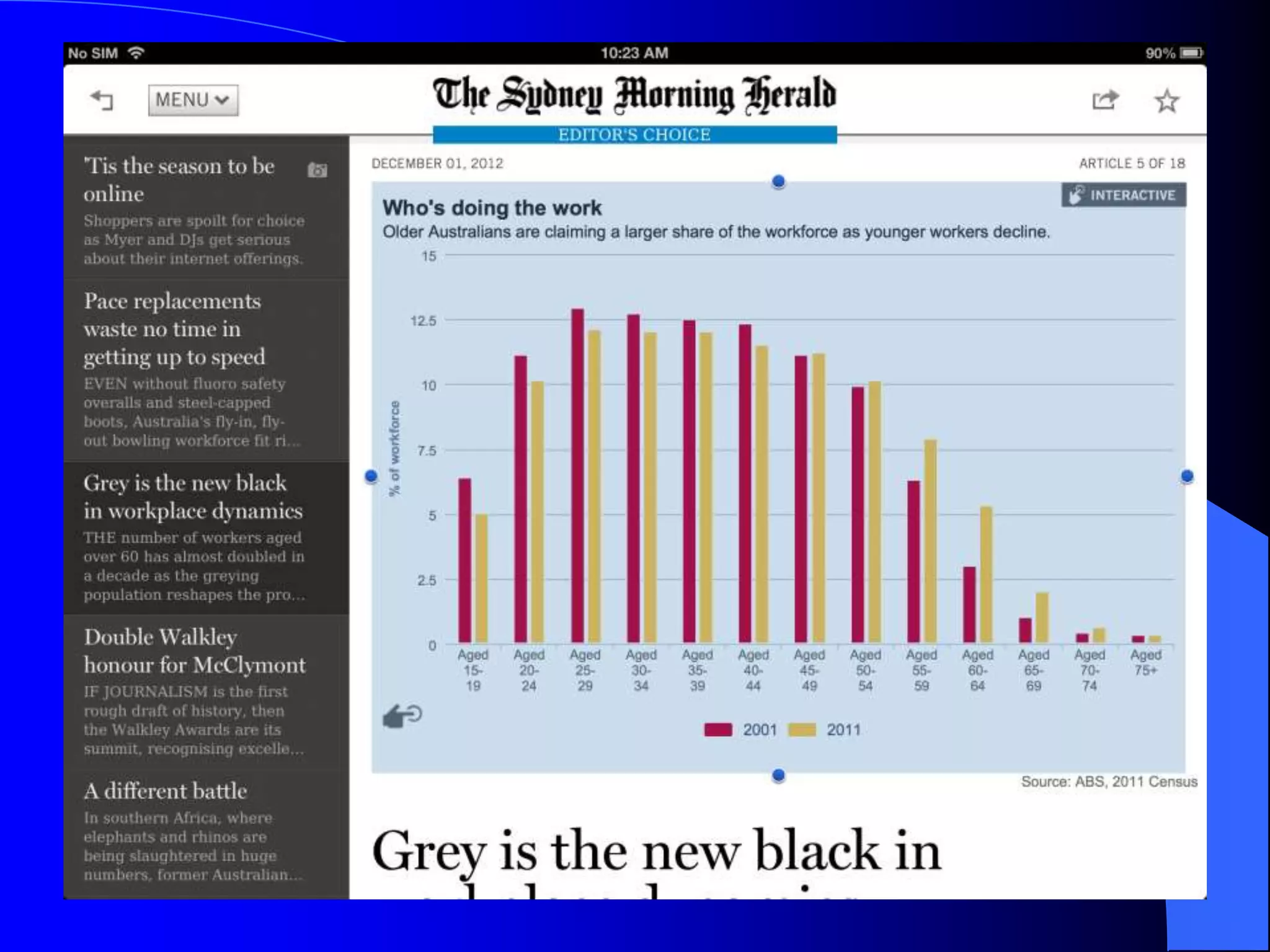
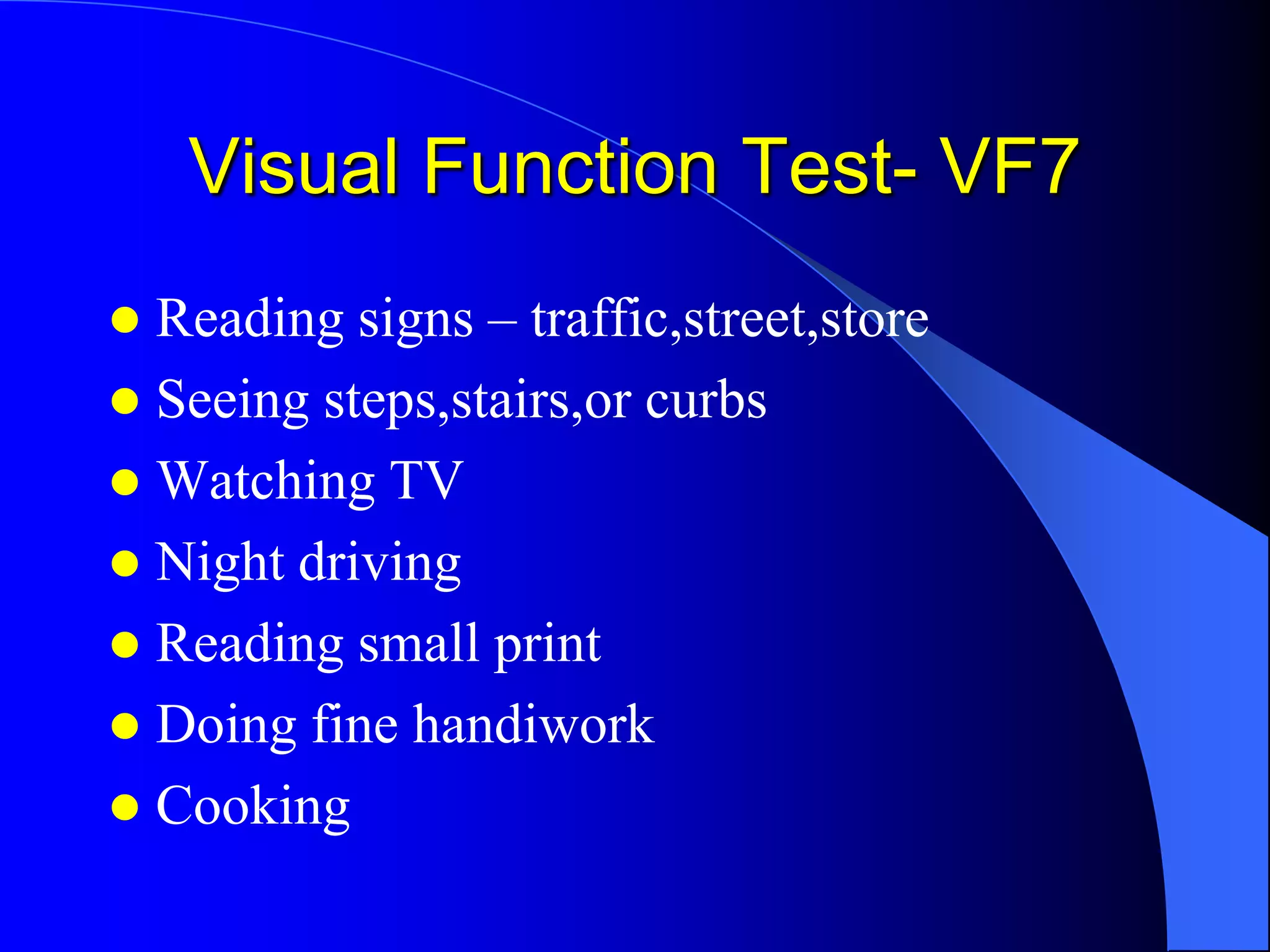
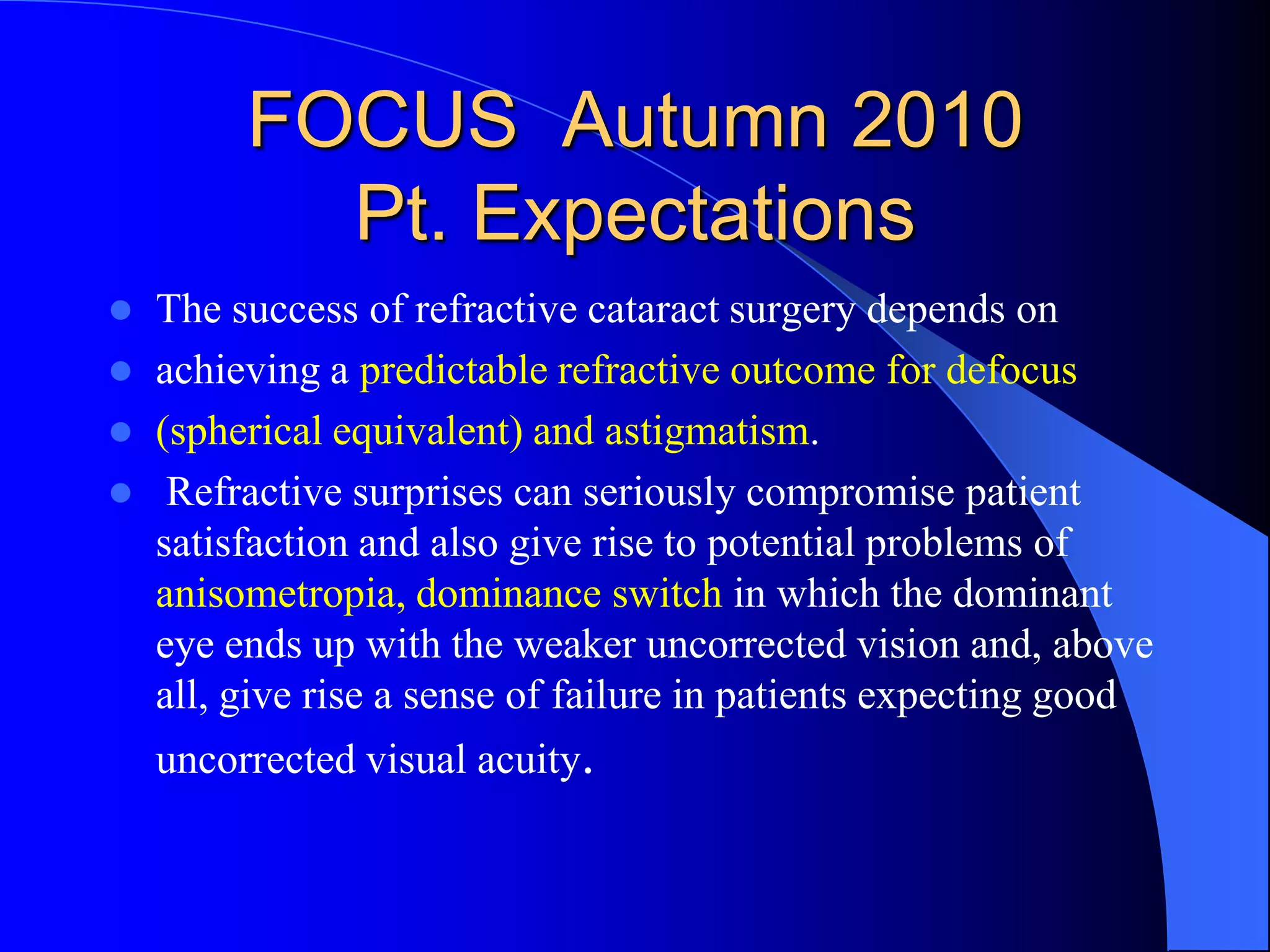
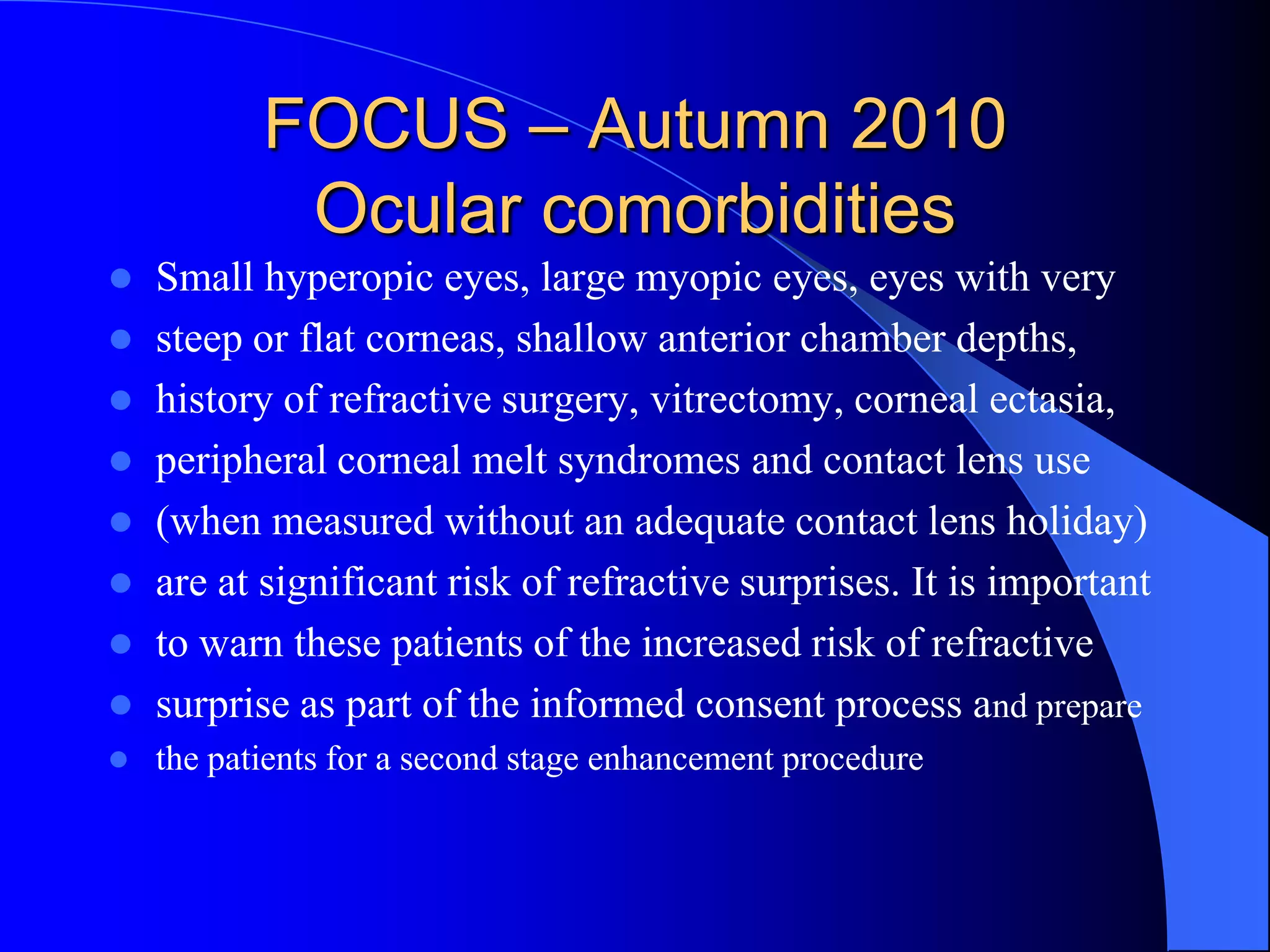
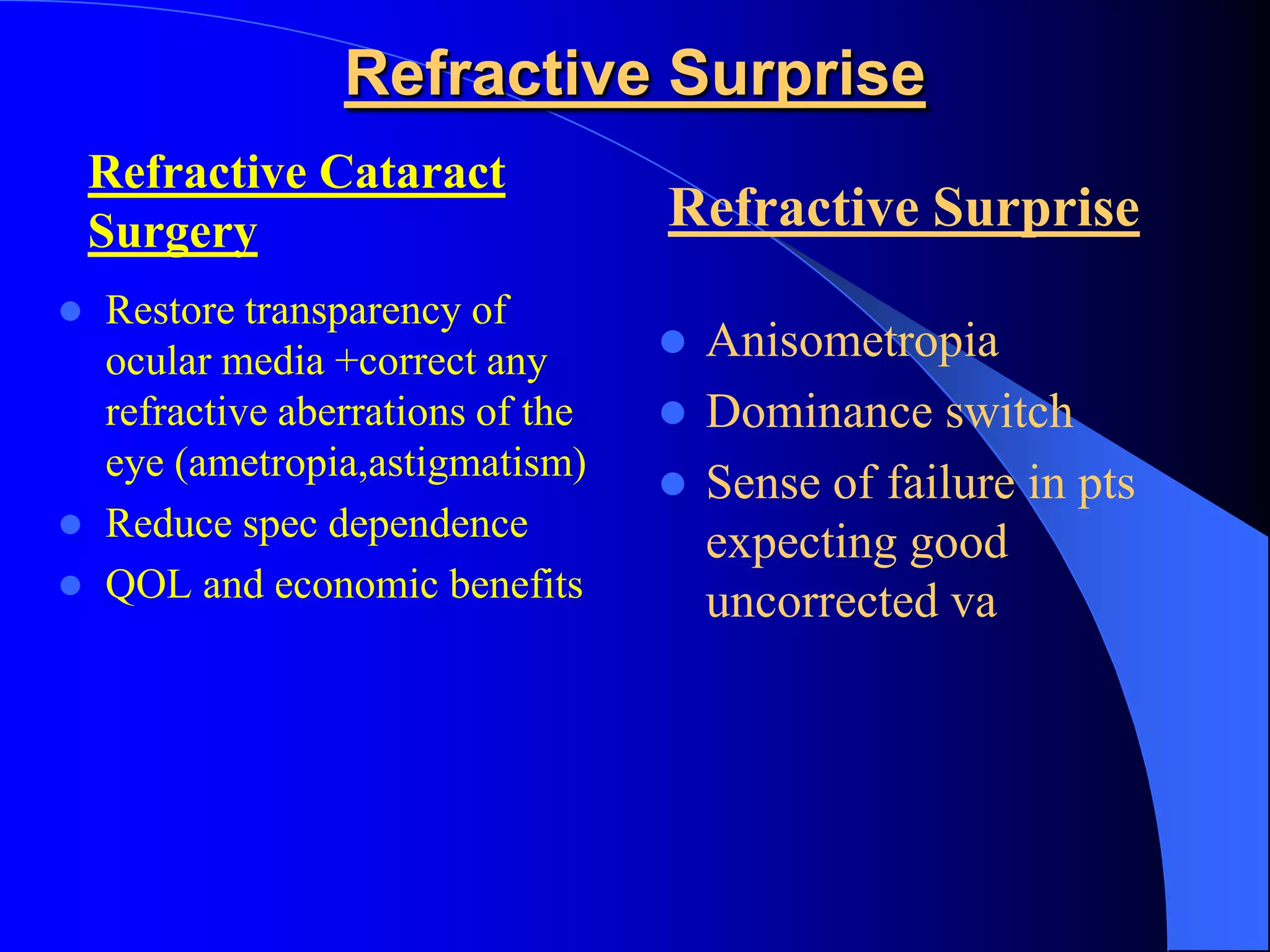
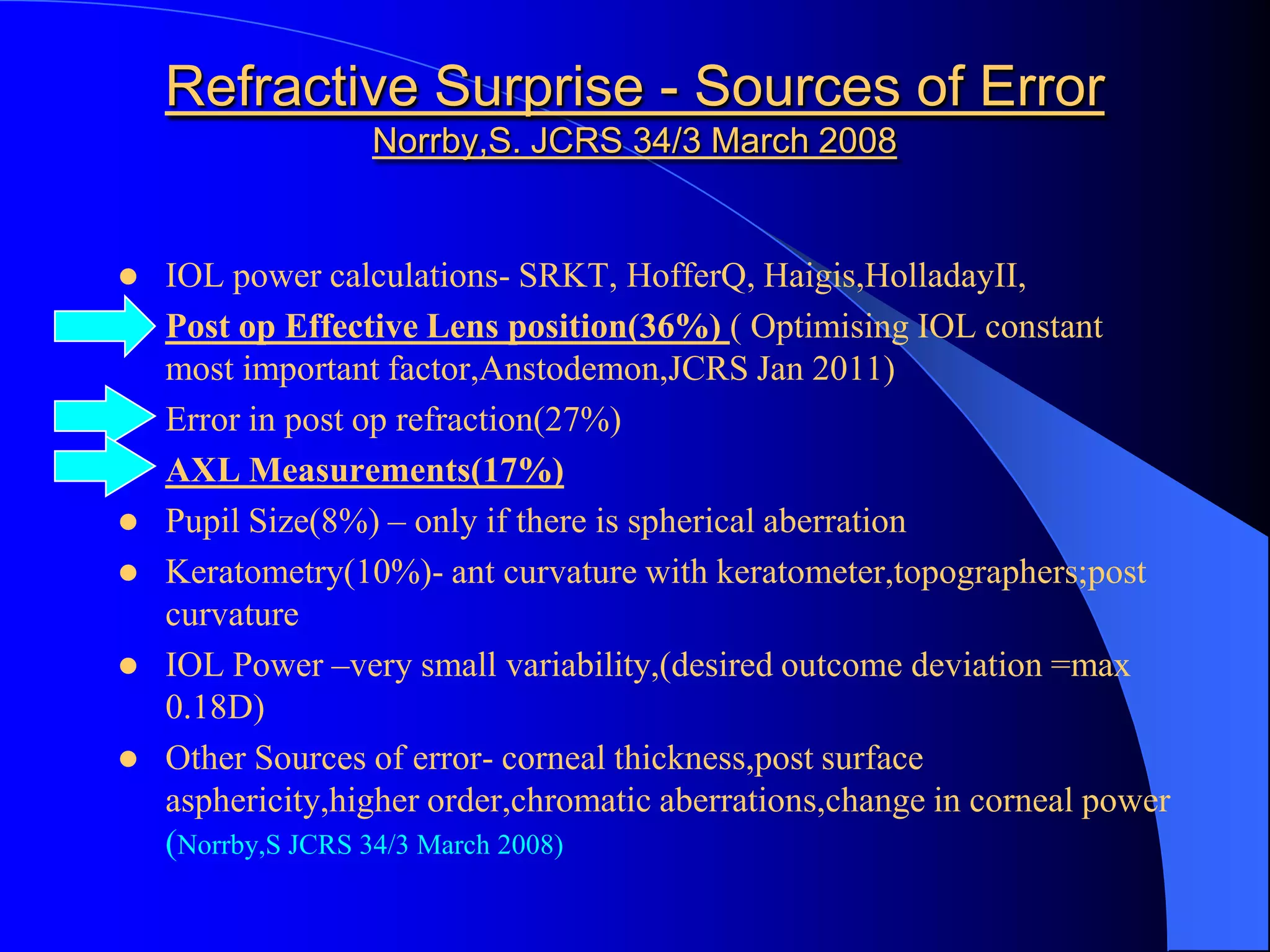
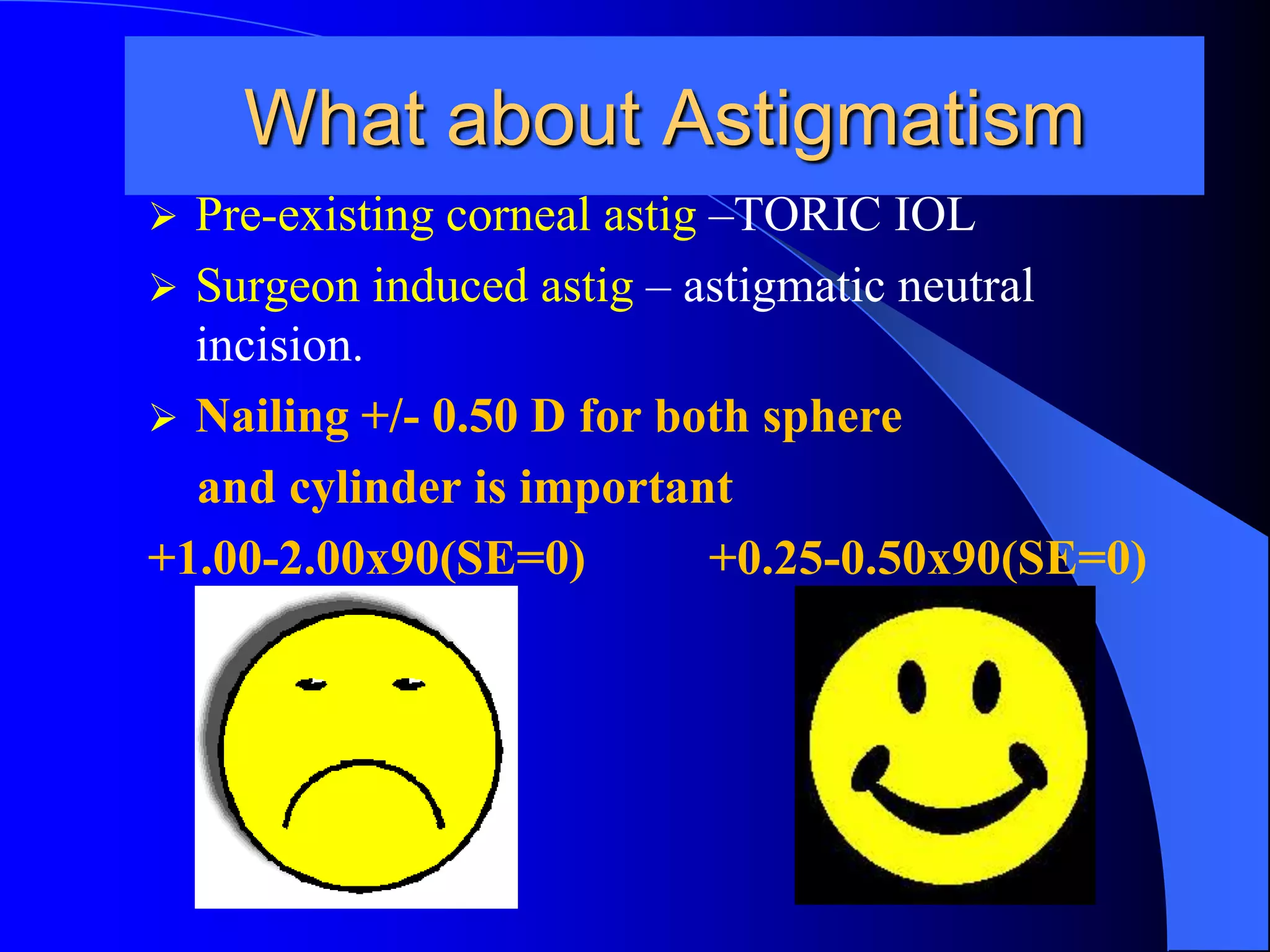
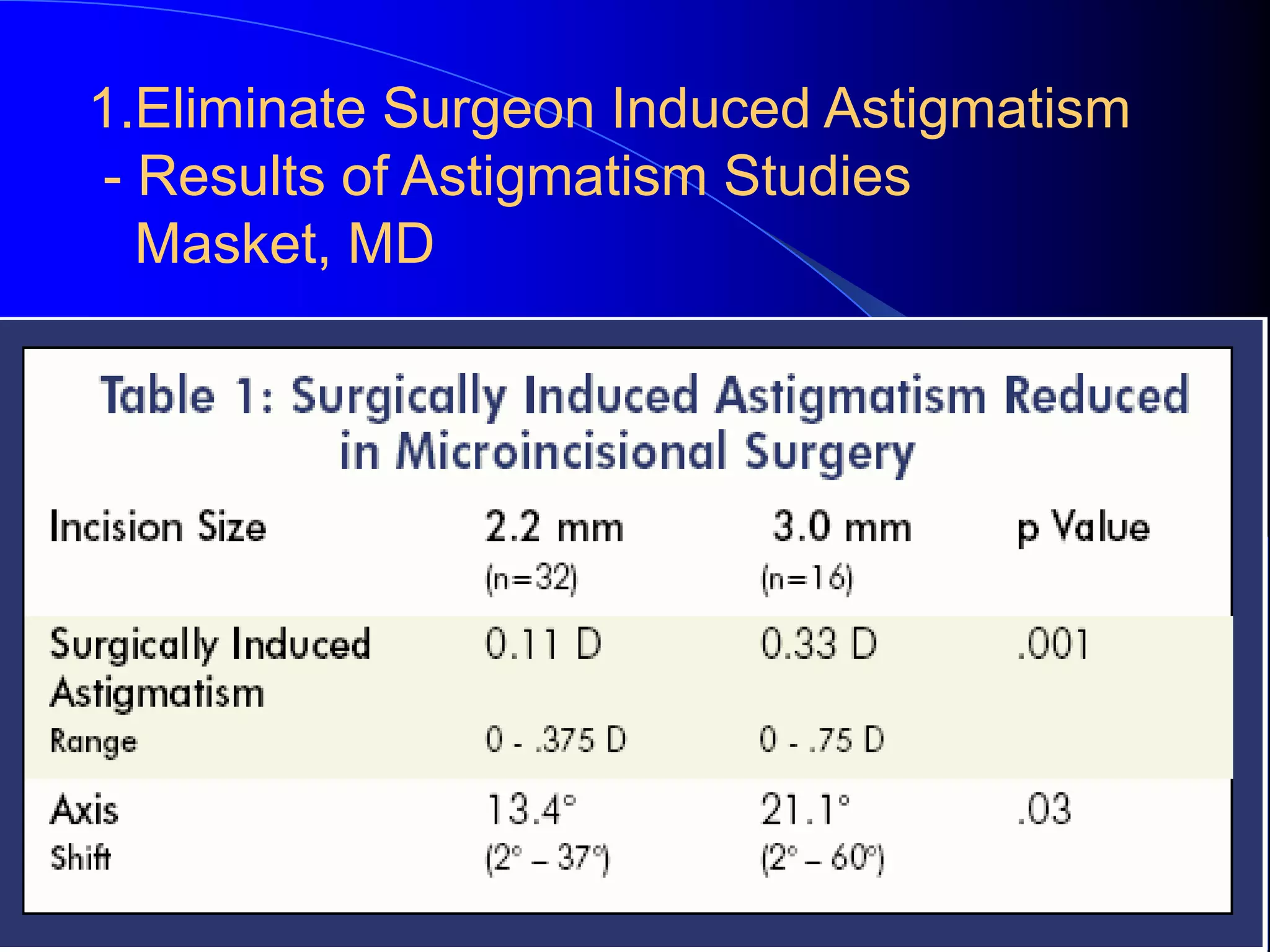
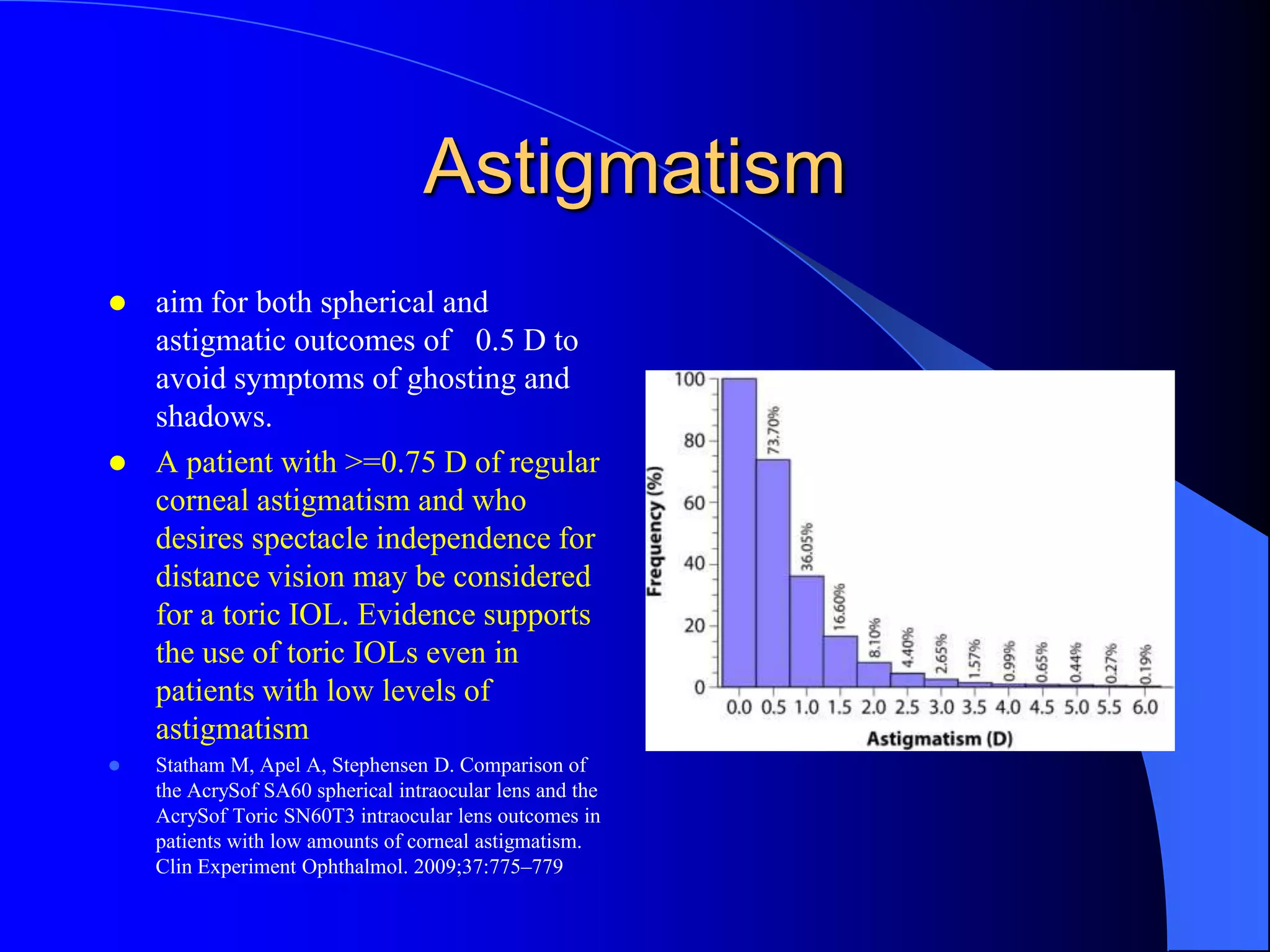
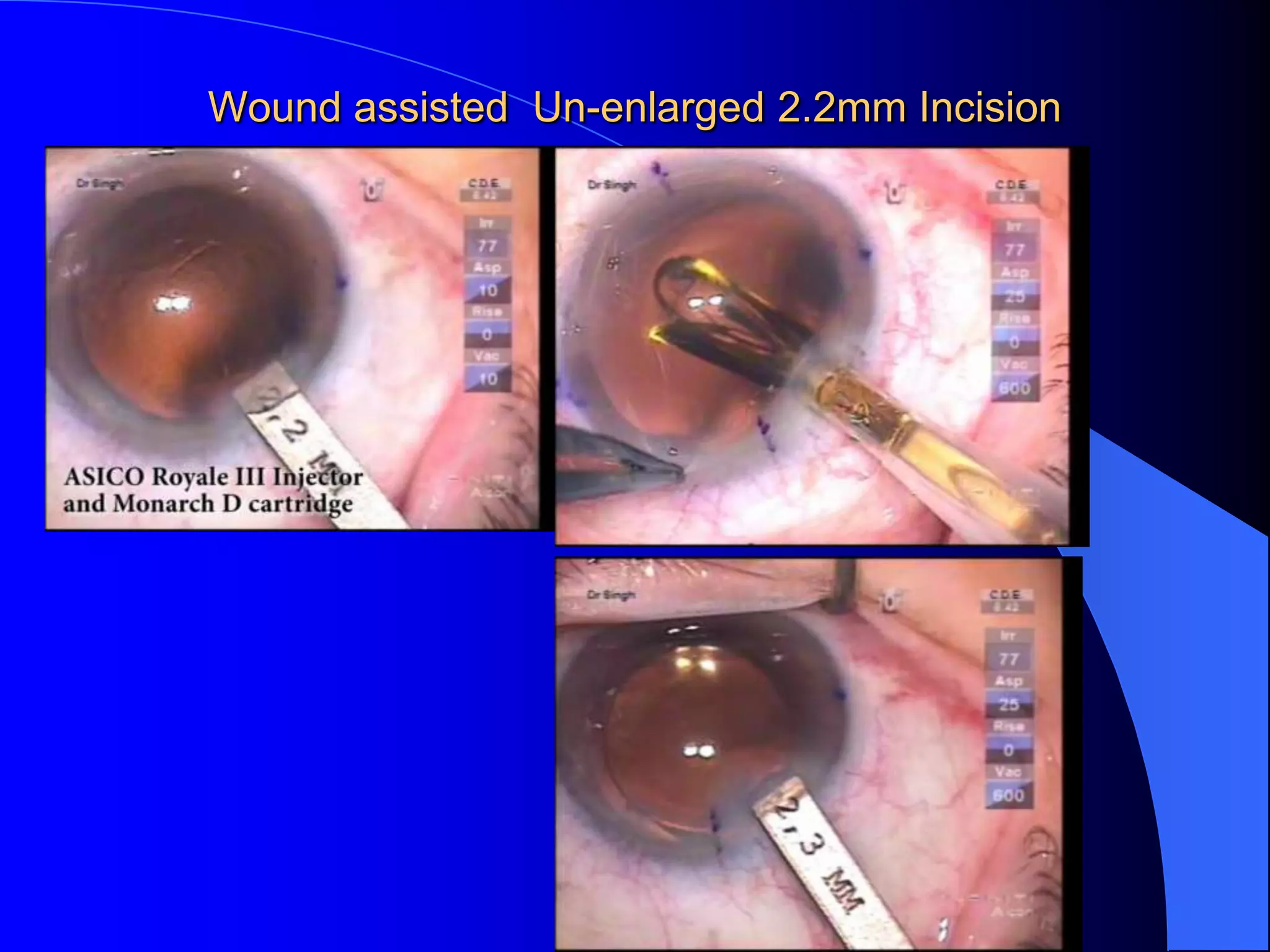
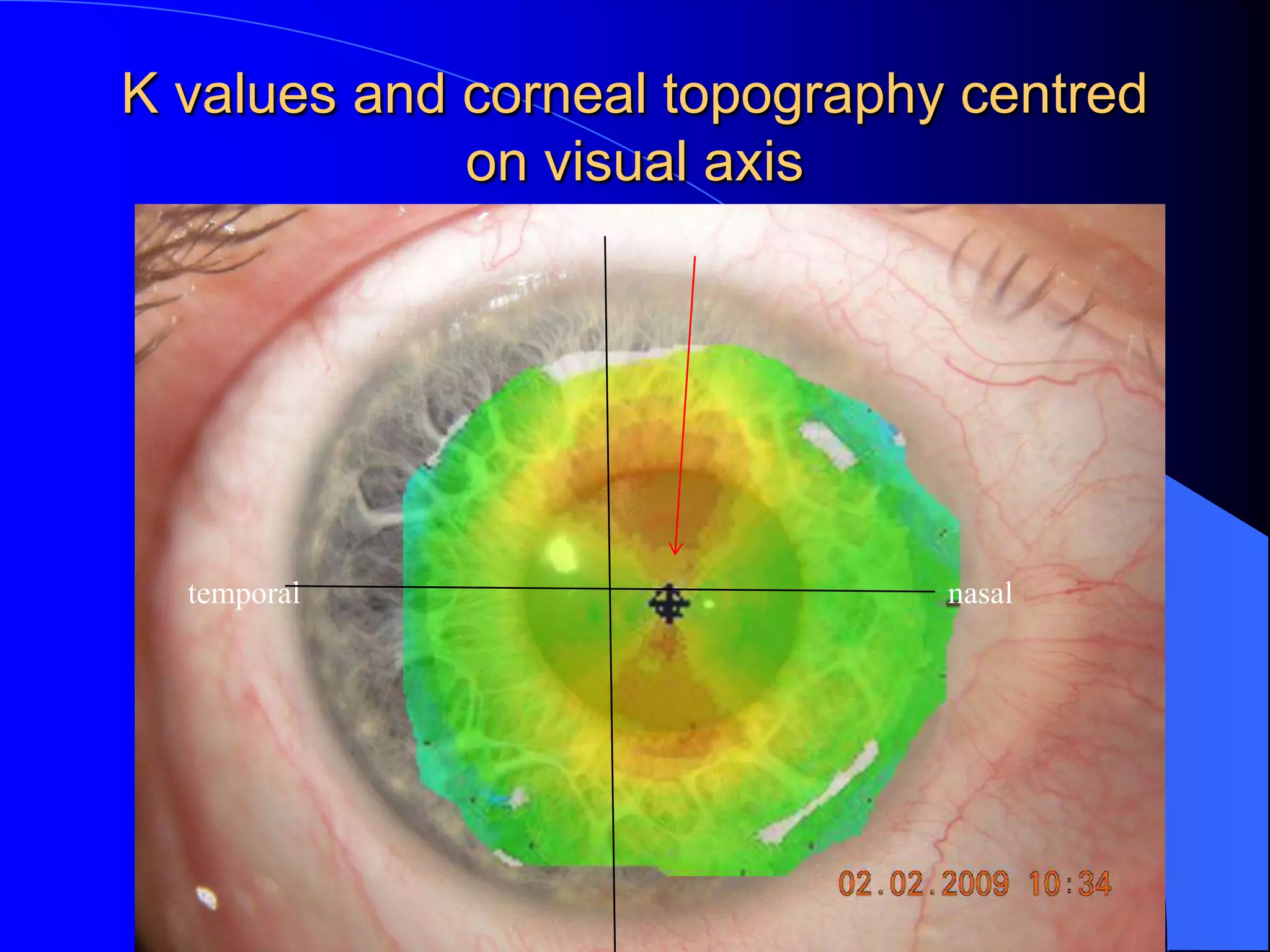
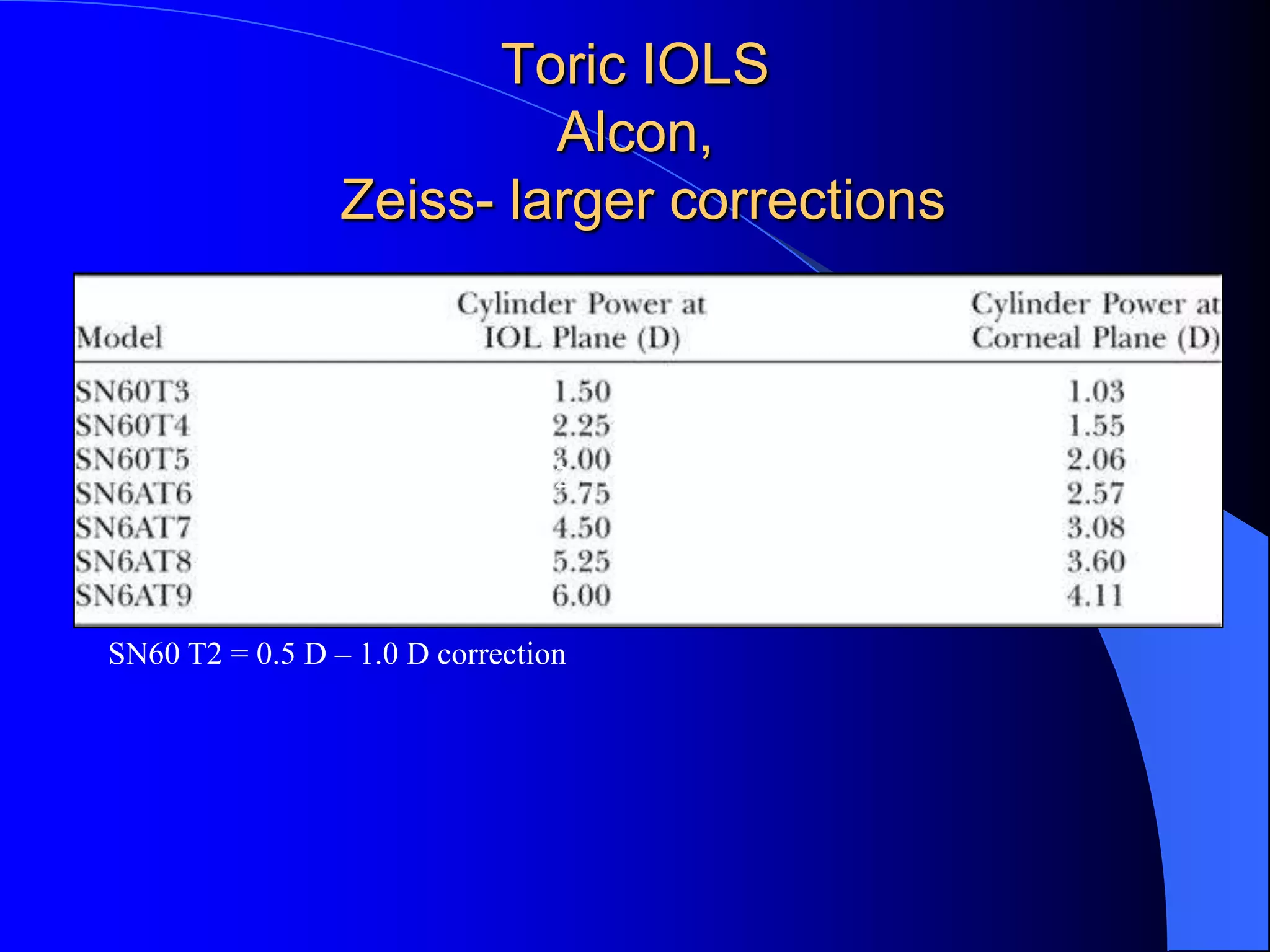
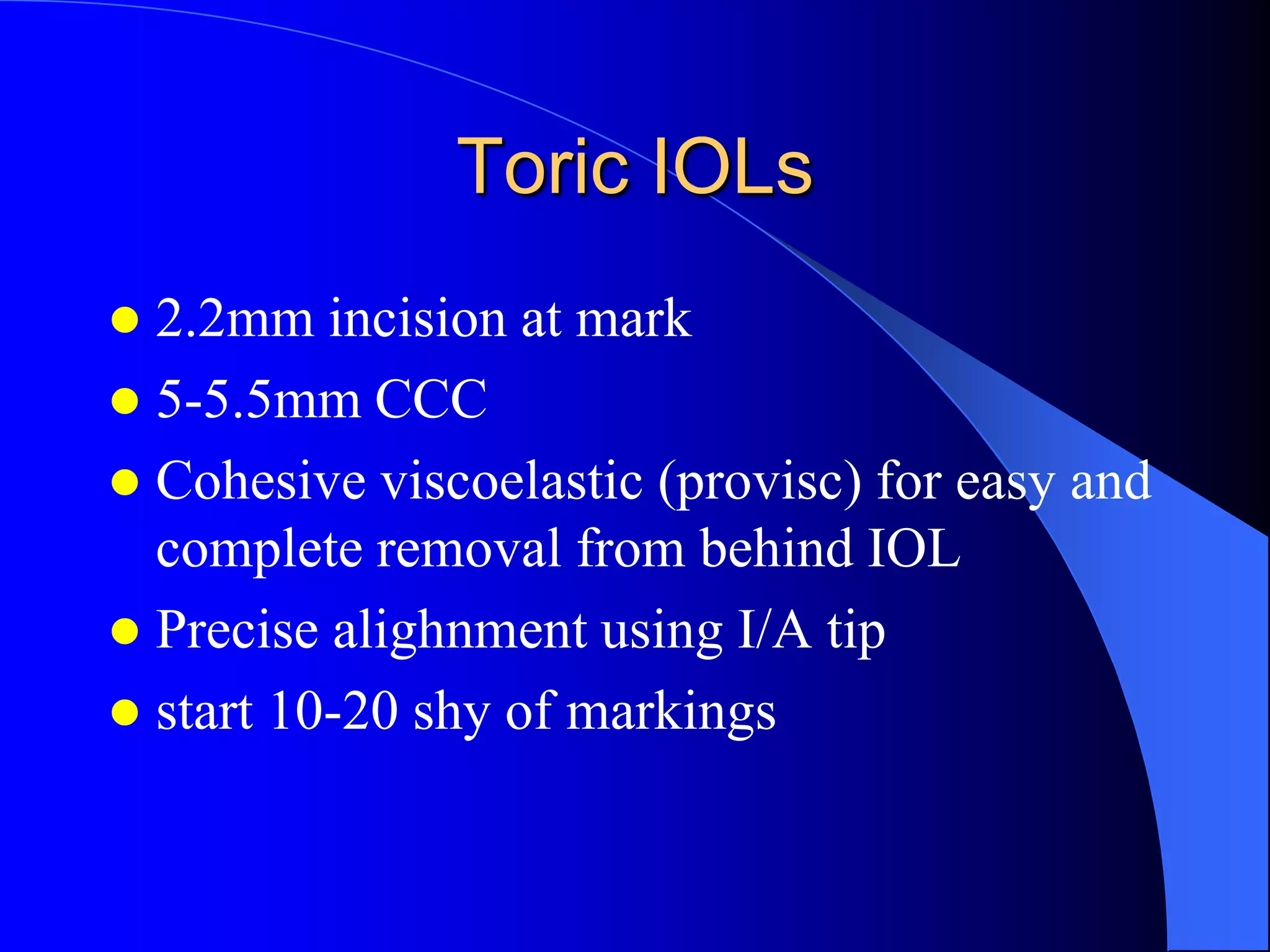
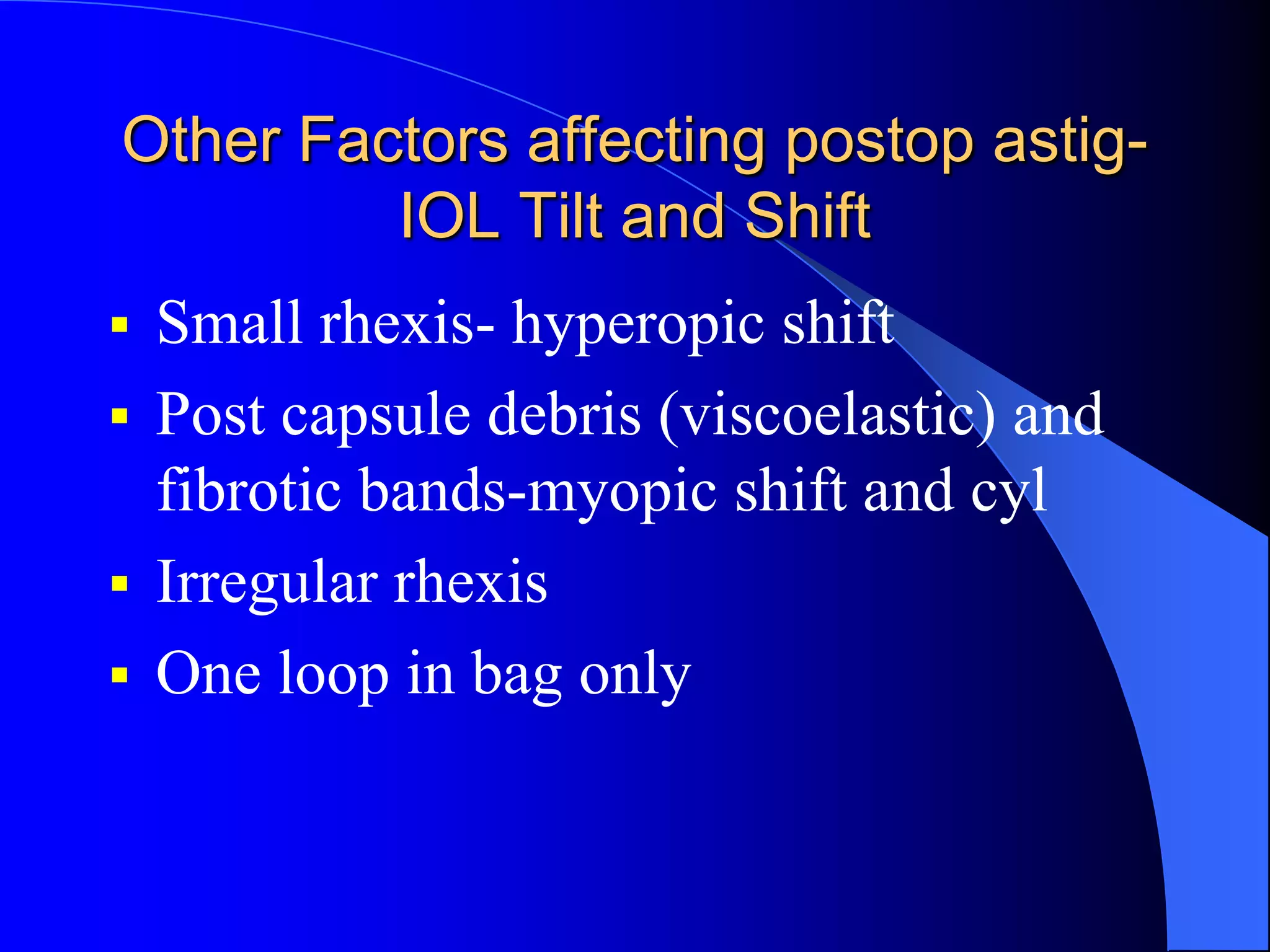
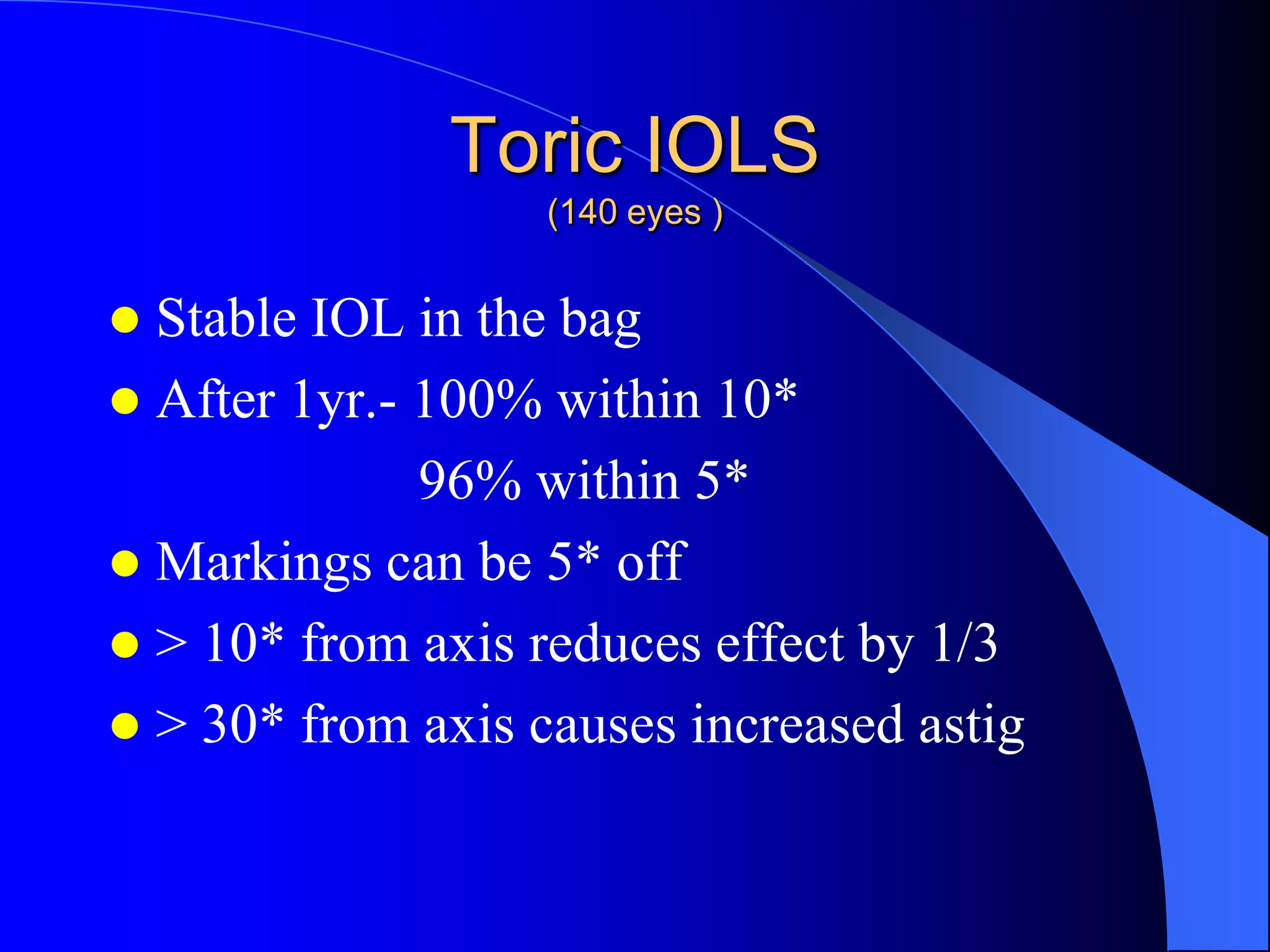
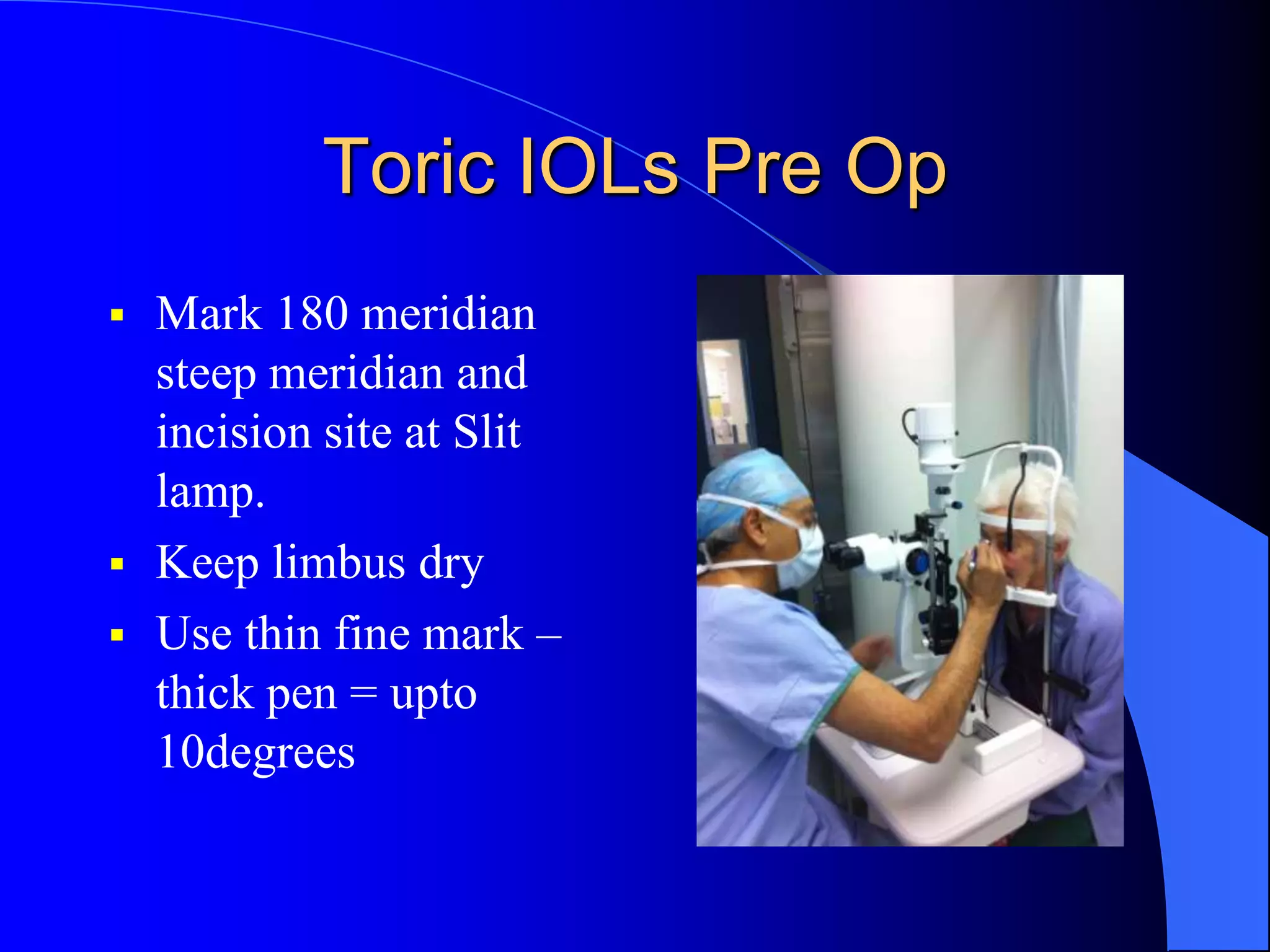
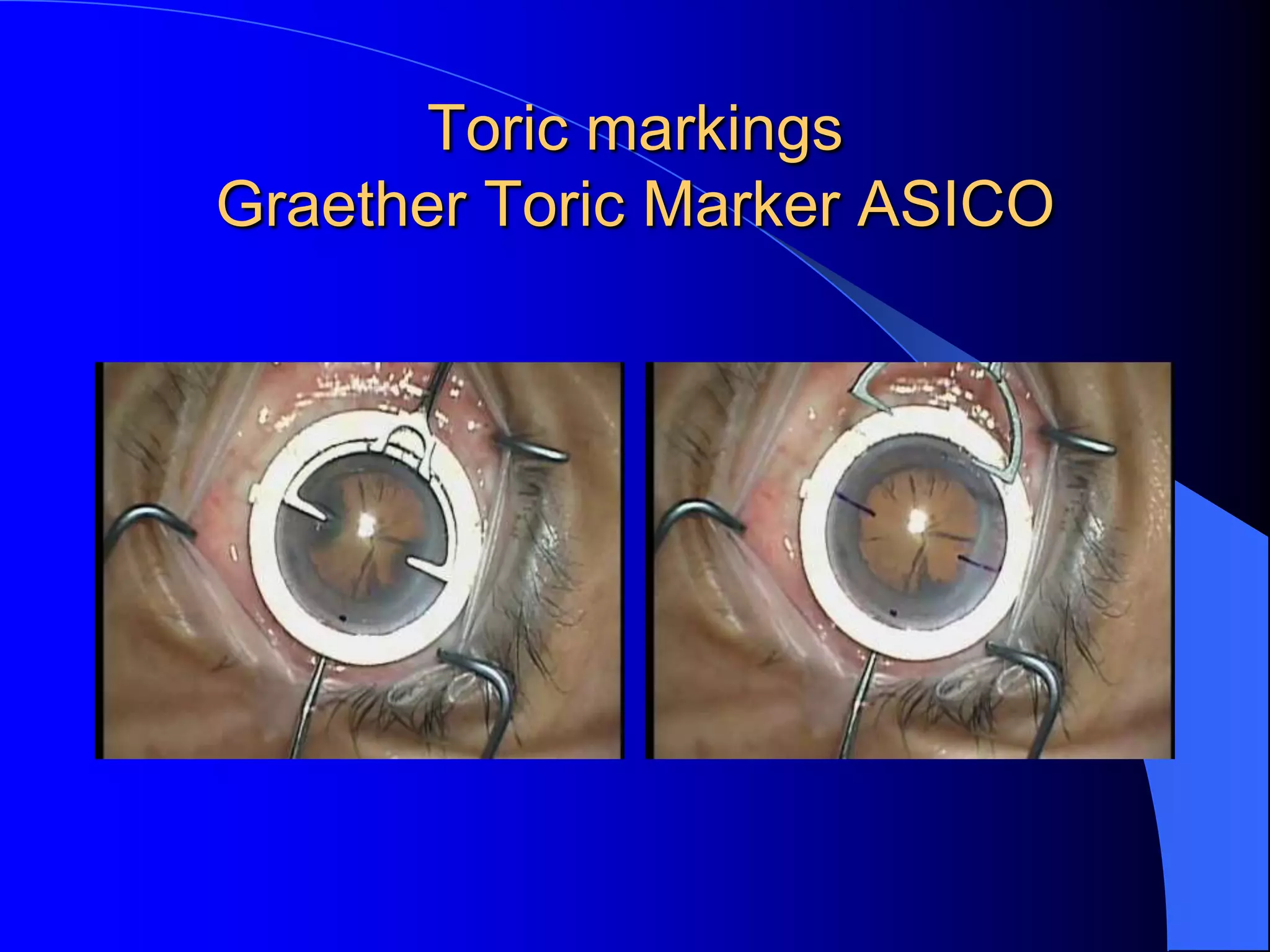
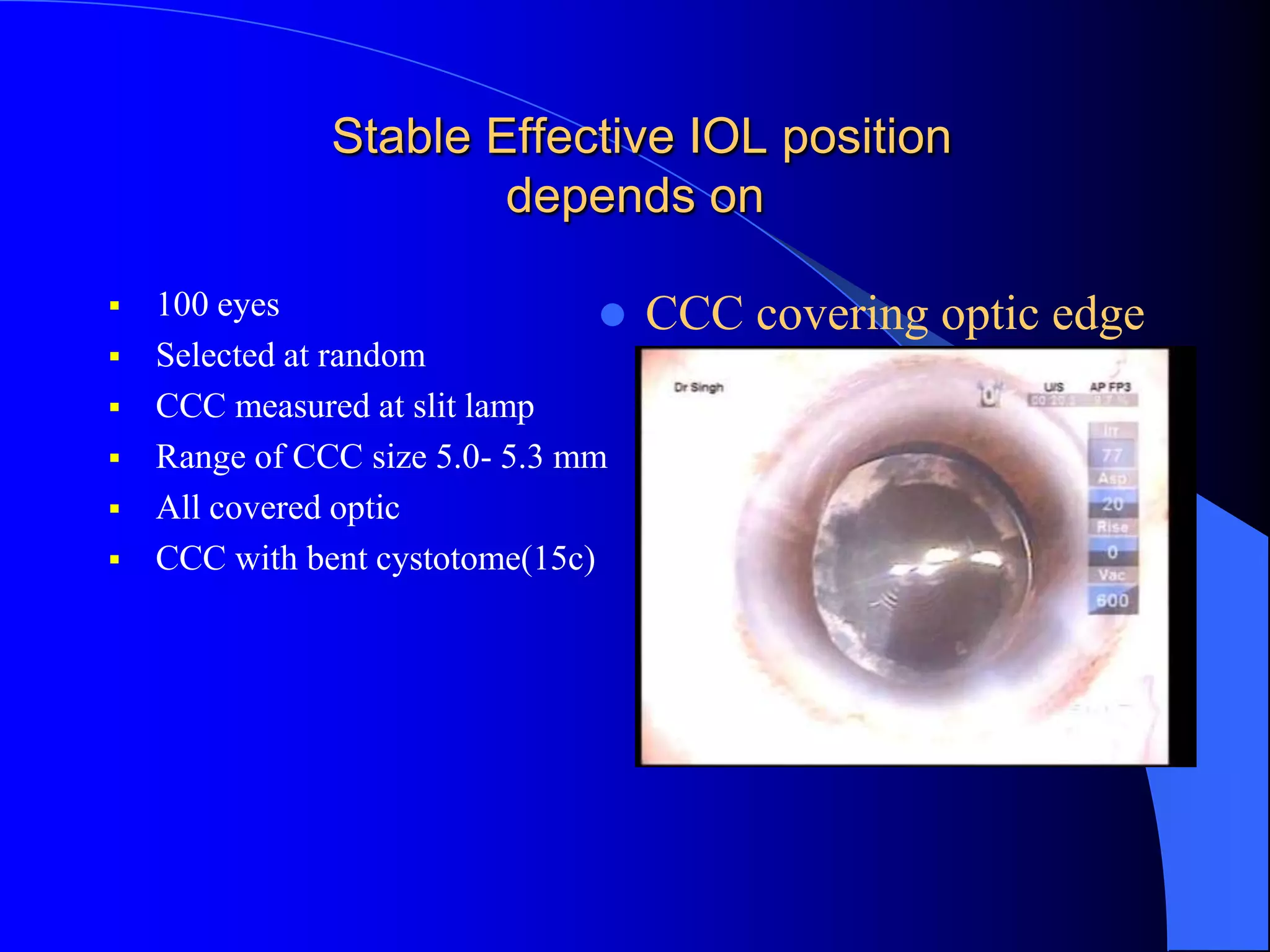
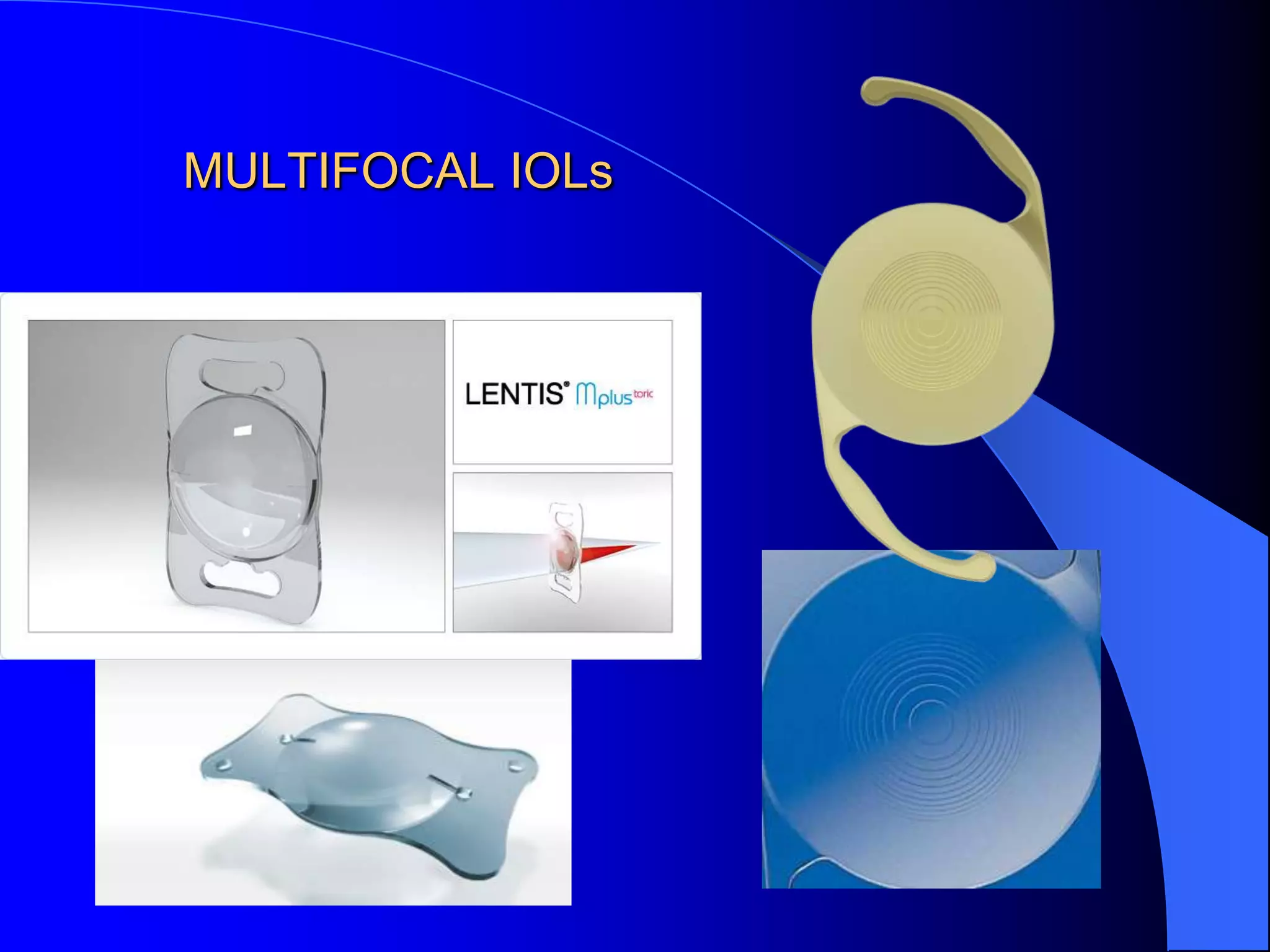
The document discusses the techniques and decision-making processes involved in modern cataract surgery, highlighting the importance of achieving optimal visual outcomes, minimizing astigmatism, and ensuring patient satisfaction. It emphasizes the role of preoperative assessments, the use of toric and multifocal intraocular lenses, and strategies to avoid refractive surprises and complications. Key factors such as surgical technique, patient health, and the specific needs of individuals are outlined to ensure successful cataract surgery results.