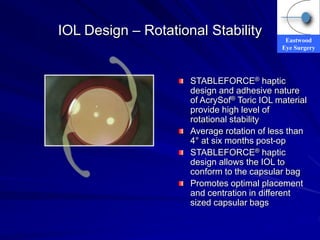
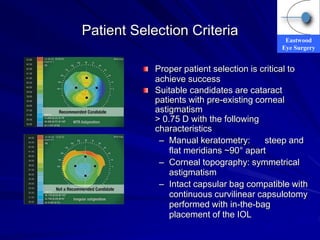
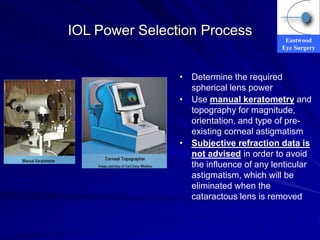
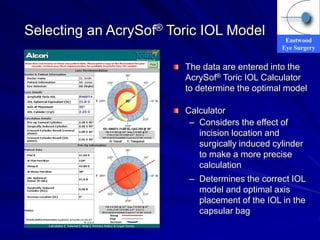
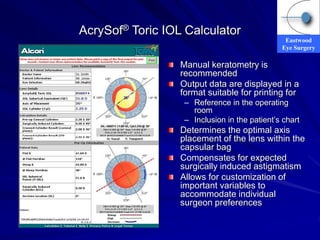
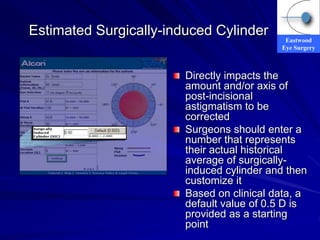
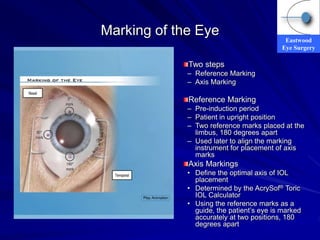
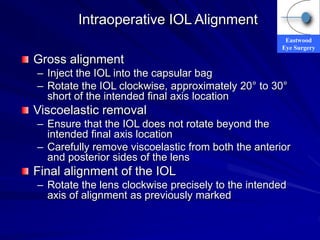
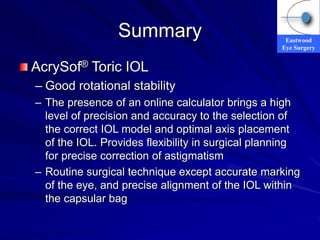
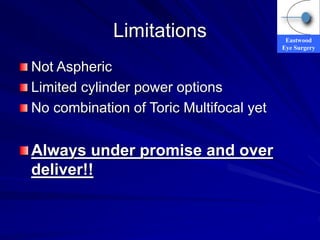
The document discusses advancements in cataract and refractive surgery, particularly focusing on toric intraocular lenses (IOLs) for correcting astigmatism. It emphasizes the importance of proper patient selection, IOL design, and surgical precision in achieving optimal outcomes, highlighting the Acrysof® toric IOL's rotational stability and the usage of a calculator for precise selection and placement. Additionally, it addresses limitations of the current technology and future directions for improving IOL designs.