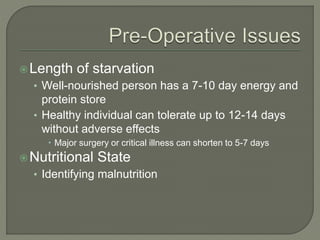
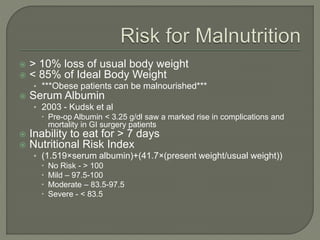
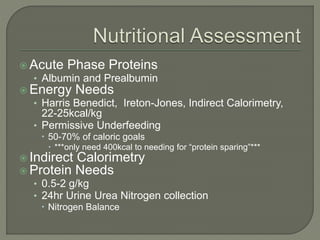
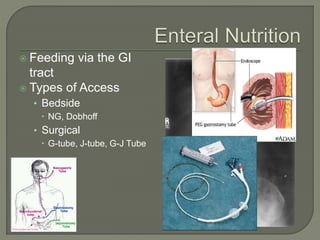
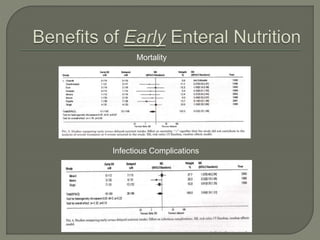
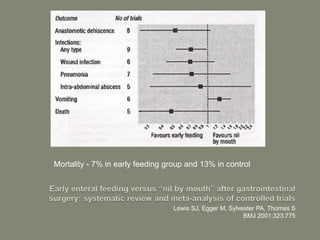
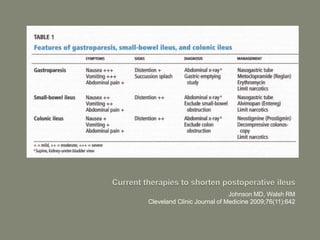
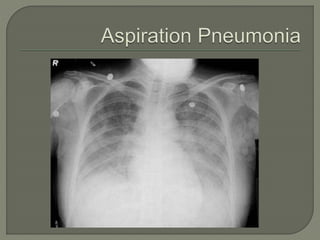
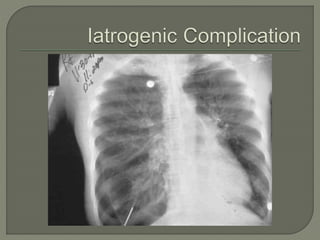
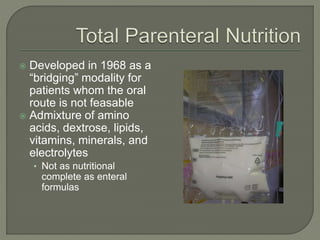
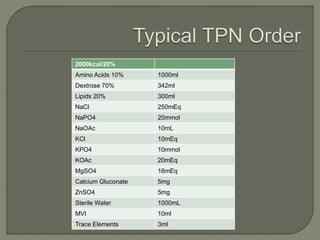
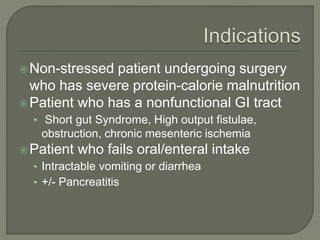
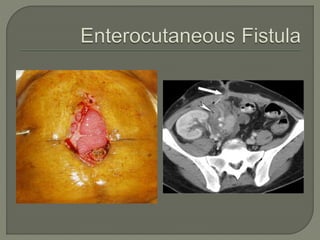
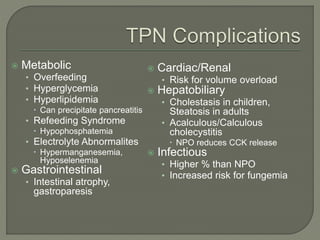
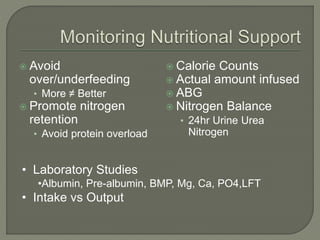
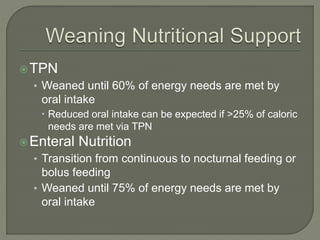
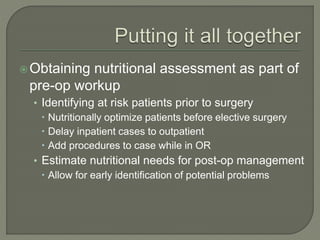
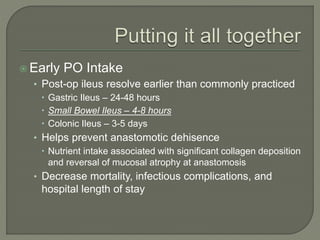
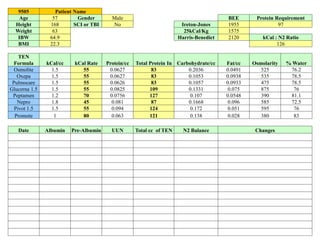
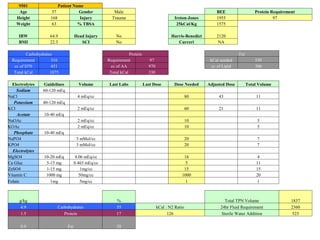
This document provides an overview of the history and clinical applications of enteral and parenteral nutrition. It discusses how ancient Egyptians used enemas to deliver nutrients and how total parenteral nutrition was developed in the 1960s. The document outlines factors to consider in determining a patient's nutritional needs such as weight loss, albumin levels, and ability to eat. Guidelines are provided for initiating and advancing enteral and parenteral nutrition based on a patient's condition and nutritional status. Potential complications of each method are also reviewed.