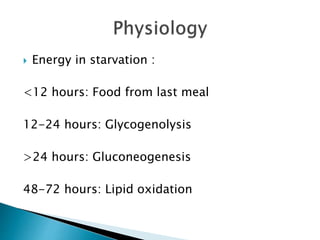
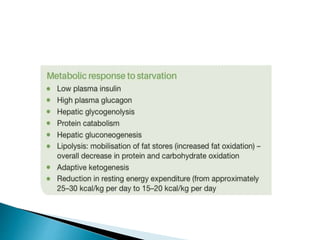
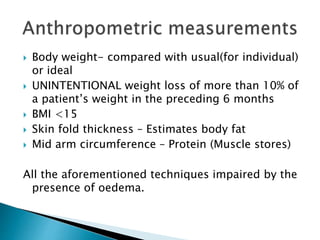
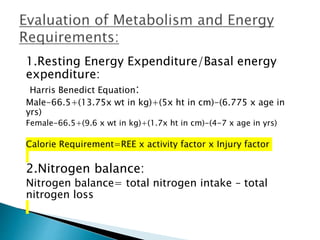
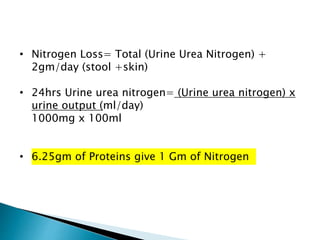
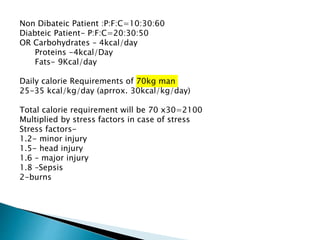
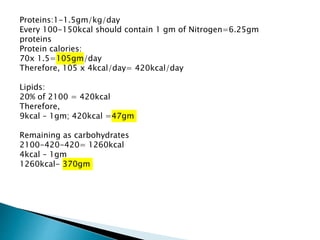
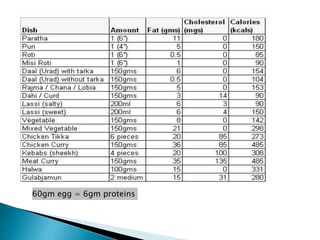
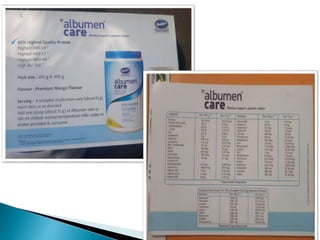
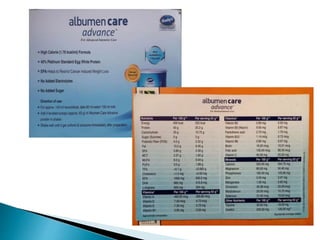
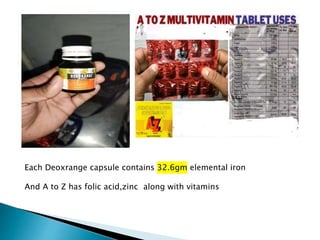
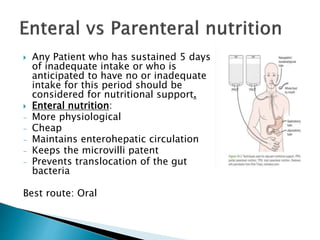
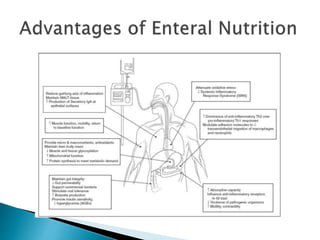
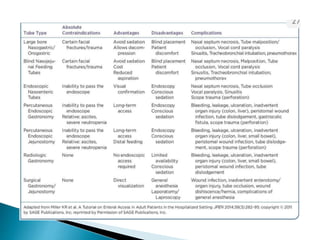
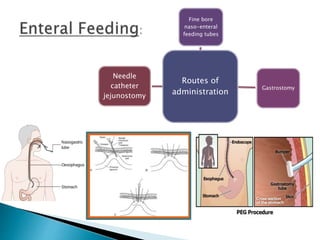
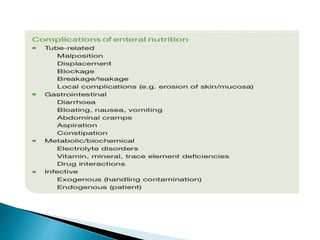
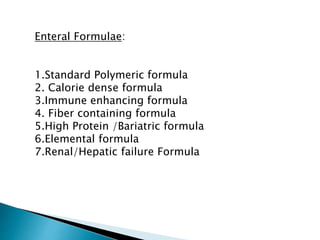
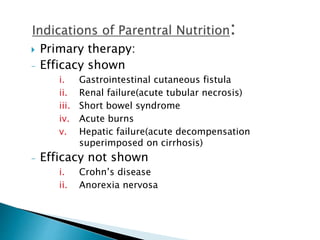
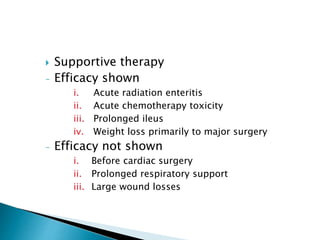
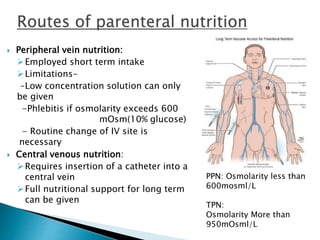
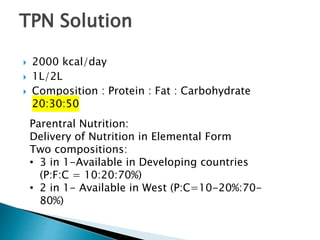
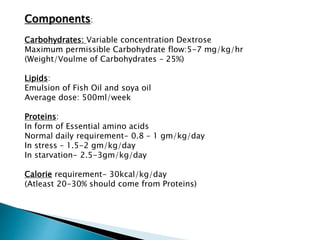
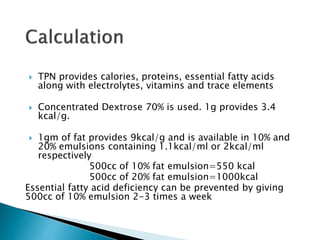
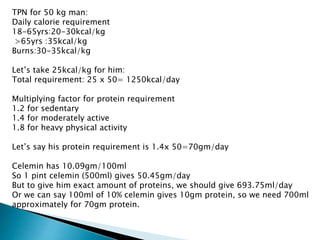
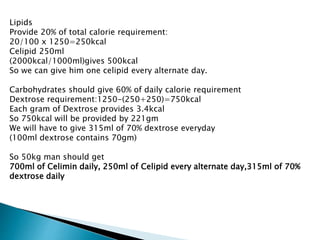
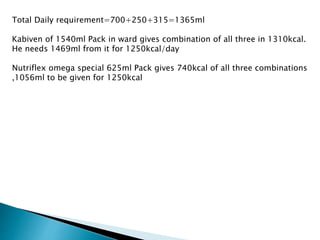
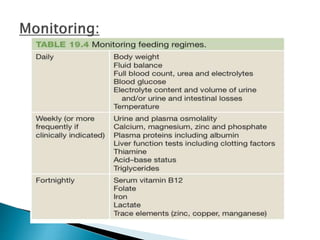
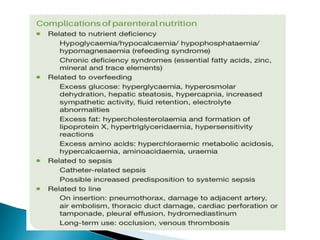
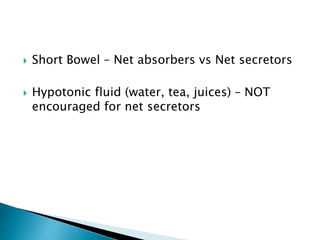
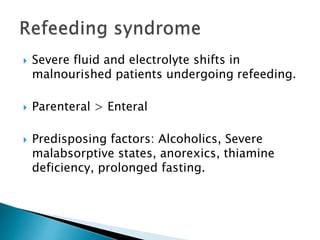
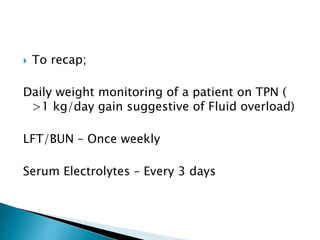
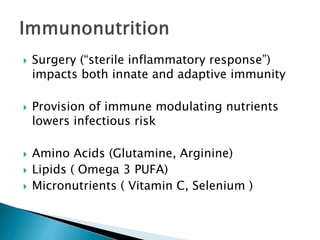
This document discusses malnutrition in surgical patients and provides guidelines on nutritional assessment and support. It notes that malnutrition is common in 30% of GI surgery patients and is often unrecognized. The aim is to identify at-risk patients and ensure their nutritional needs are met. It provides details on evaluating nutritional status, calculating calorie and protein requirements, and enteral and parenteral nutrition support options. The appropriate use of nutrition therapy is emphasized to prevent complications and support recovery from illness or surgery.