Dr. Asif Mian Ansari presented on nutritional requirements for surgical patients. Major points included:
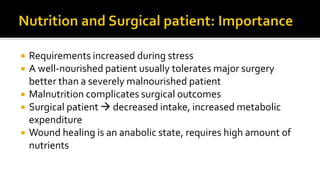
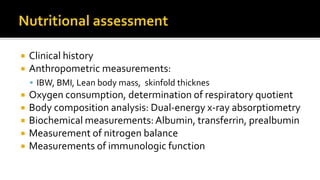
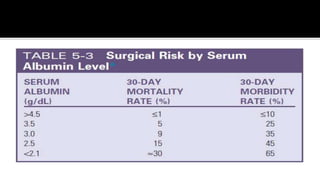
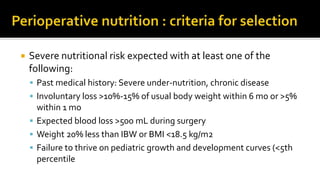
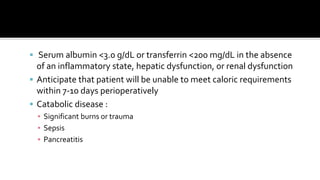
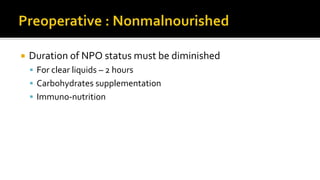
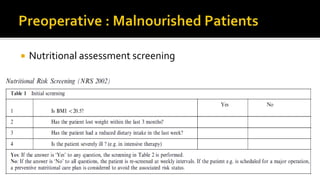
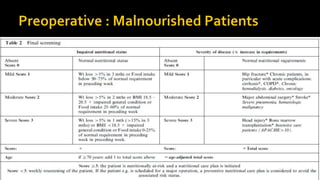
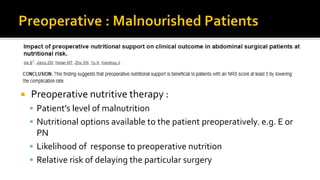
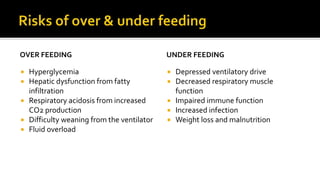
1) Malnutrition can complicate surgical outcomes as nutritional needs are increased during stress and recovery requires an anabolic state.
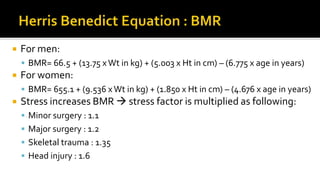
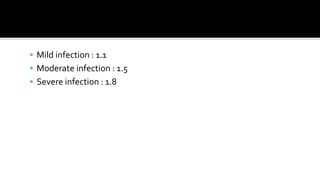
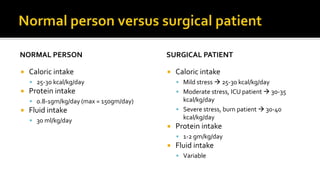
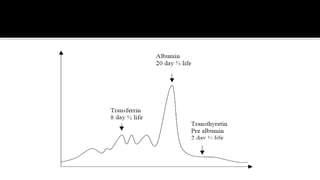
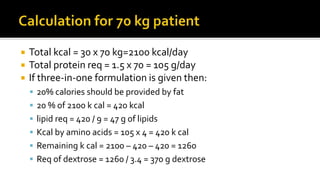
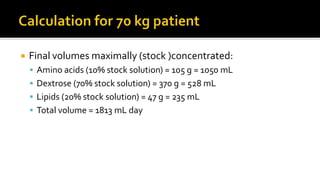
2) Formulas to calculate basal metabolic rate and increased needs during stress or infection were provided.
3) Guidelines for caloric and protein intake for normal and surgical patients depending on stress level were outlined.
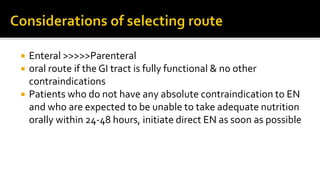
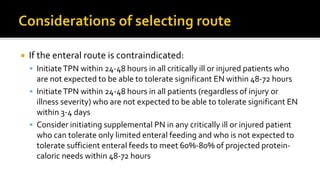
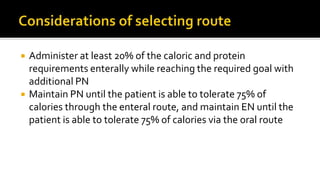
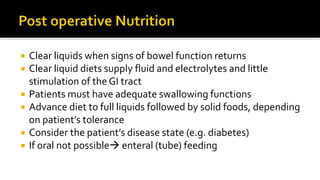
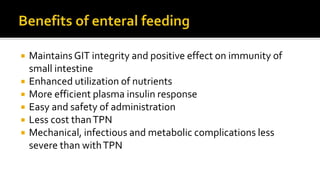
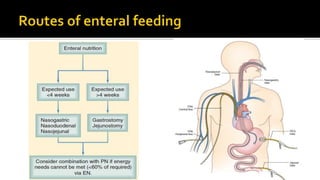
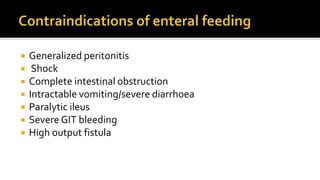
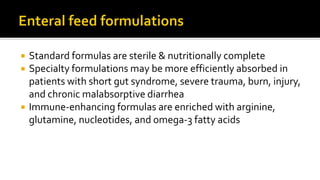
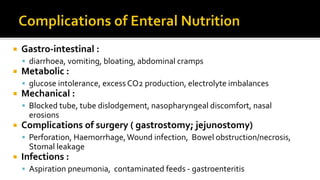
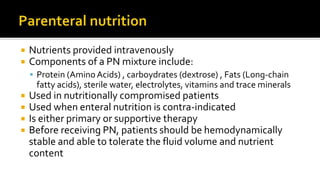
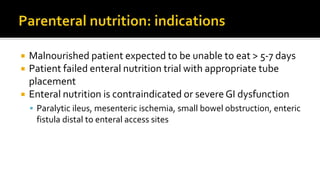
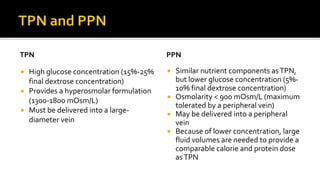
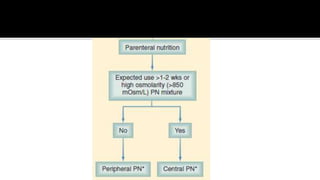
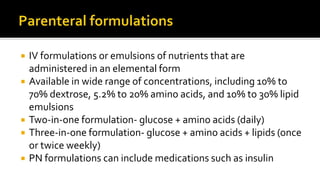
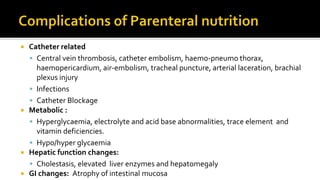
4) Enteral nutrition is preferred over parenteral nutrition when possible due to lower risk of complications.