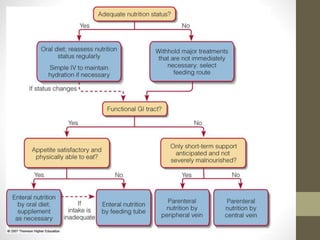
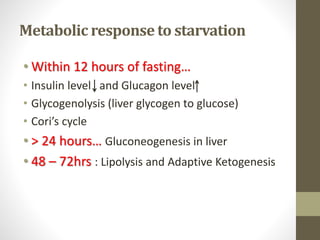
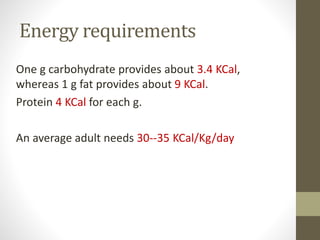
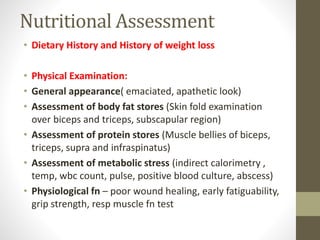
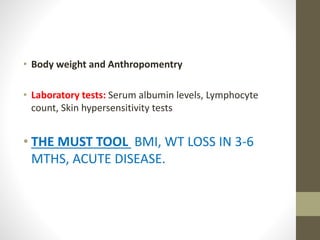
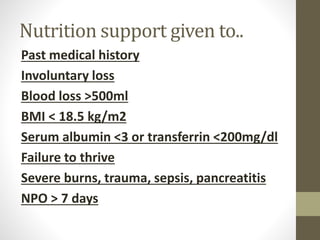
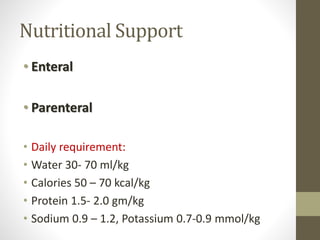
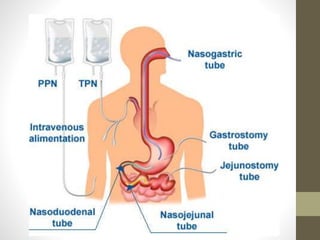
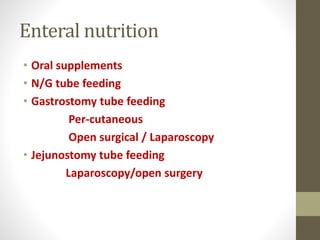
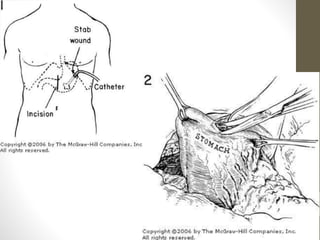
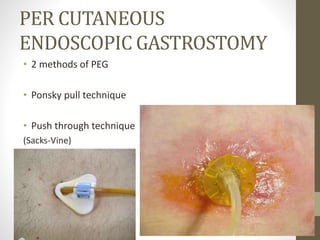
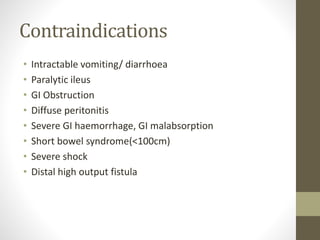
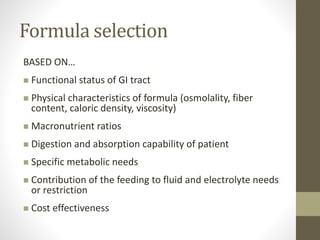
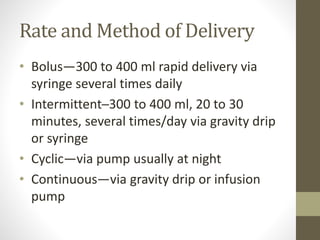
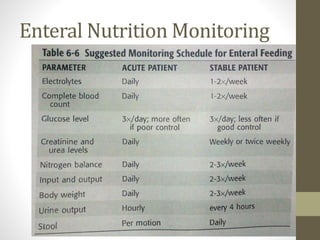
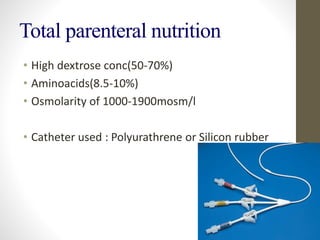
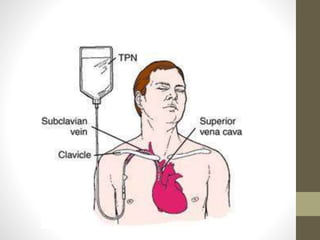
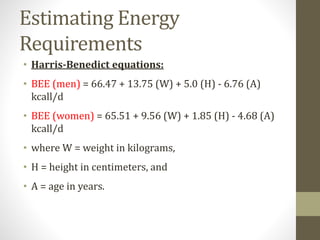
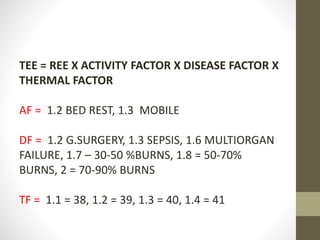
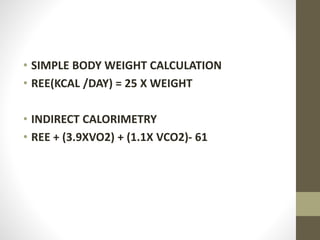
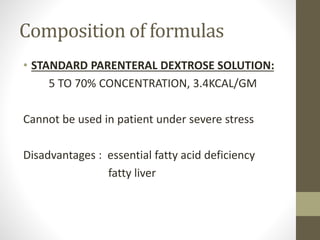
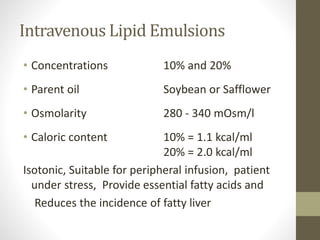
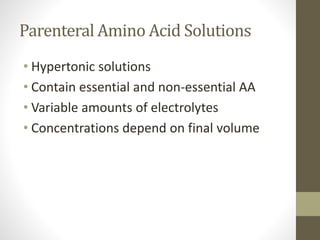
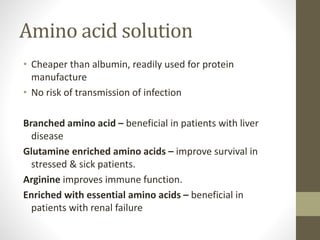
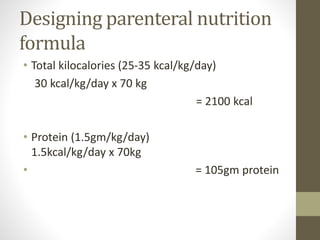
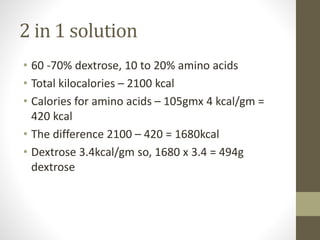
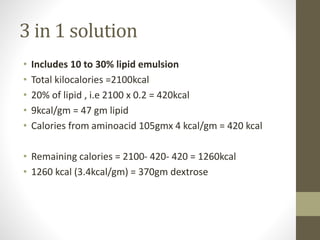
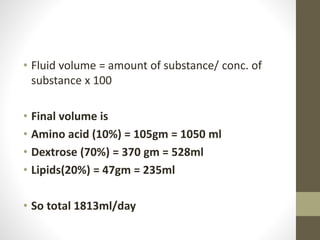
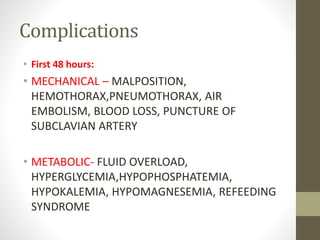
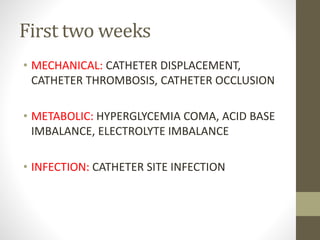
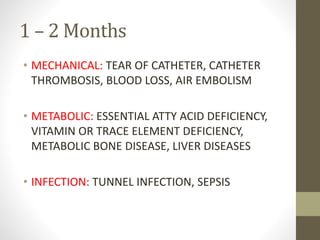
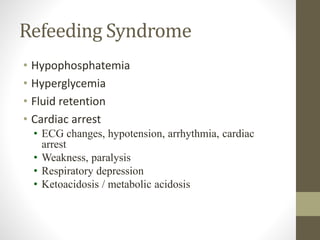
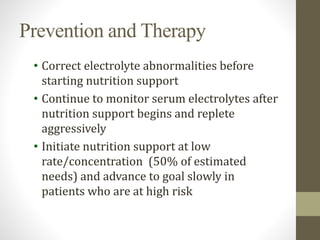
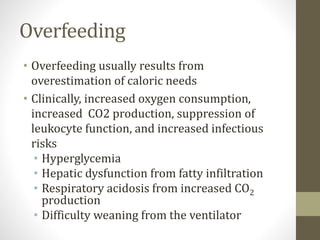
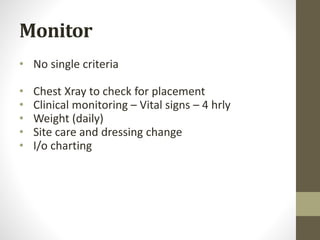
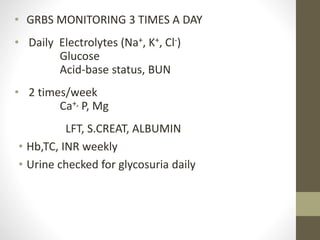
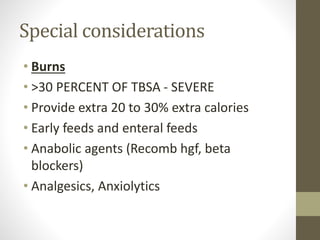
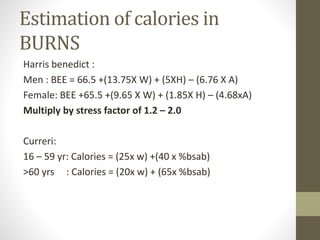
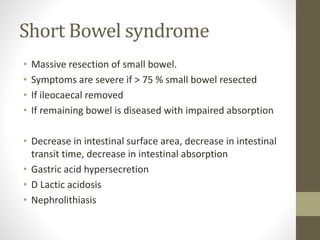
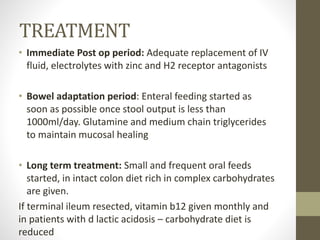
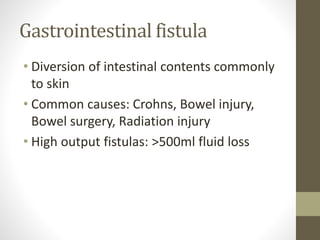
This document discusses nutrition support in surgery patients. It begins by outlining the aims of nutrition support to identify and meet the nutritional needs of at-risk patients. It then covers metabolic responses to starvation, increased energy and nutrient requirements in trauma/sepsis patients, methods of nutritional assessment, and factors that warrant nutrition support. The document provides details on enteral and parenteral nutrition support, including formulas, delivery methods, monitoring, and complications. It also addresses special considerations for burns patients and those with short bowel syndrome.