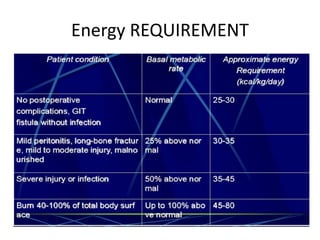
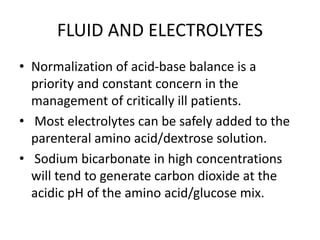
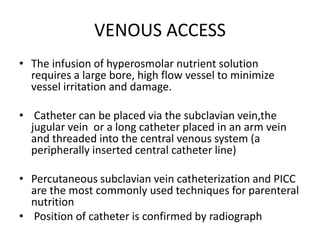
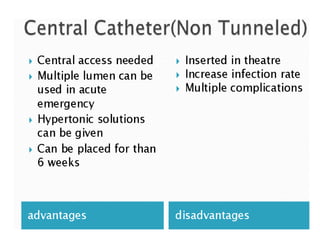
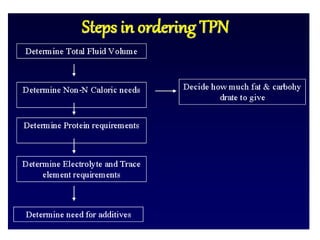
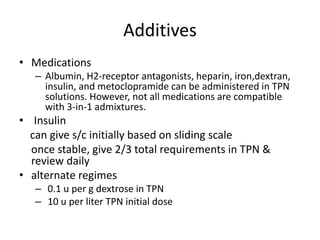
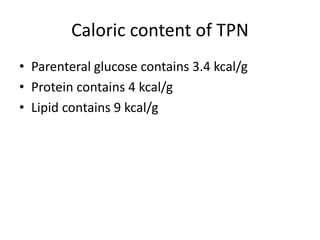
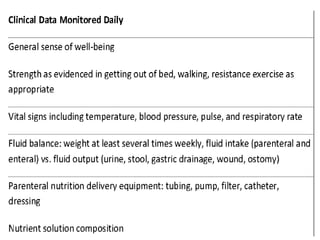
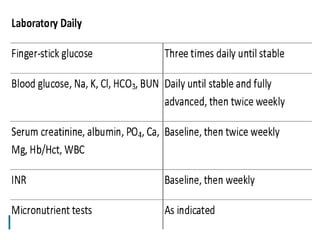
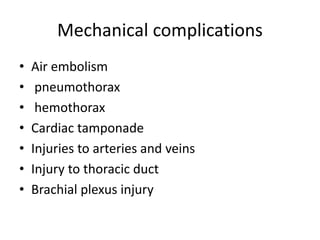
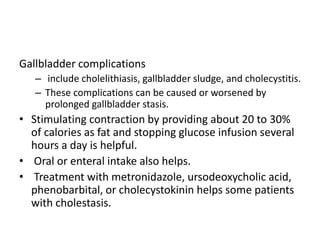
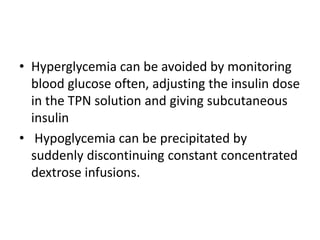
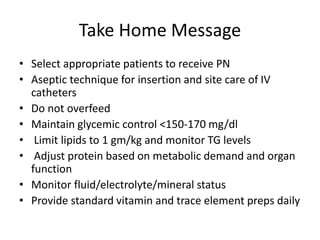
The document outlines total parenteral nutrition (TPN), its indications, contraindications, and nutritional components necessary for patients unable to meet their dietary needs through oral or enteral feeding. It discusses both adult and pediatric indications, various formulations and their administration methods, as well as monitoring and potential complications of TPN. Overall, TPN aims to provide all essential nutrients intravenously to support patients with severe gastrointestinal dysfunction or other specific medical conditions.