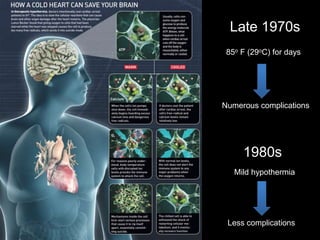
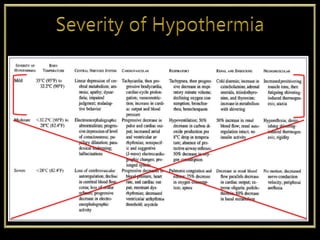
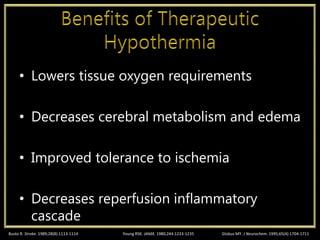
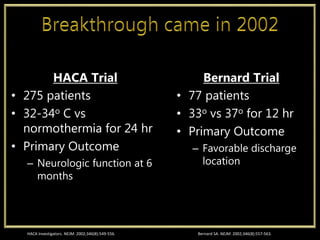
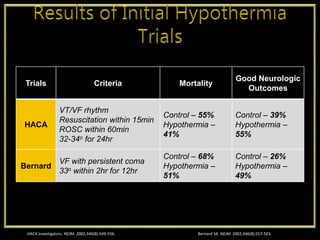
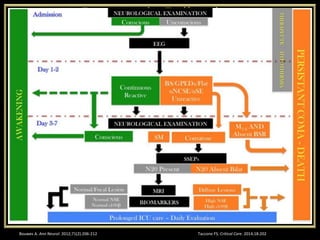
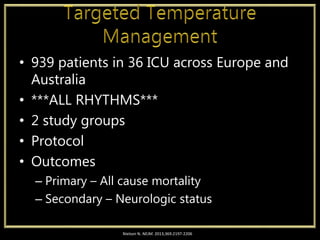
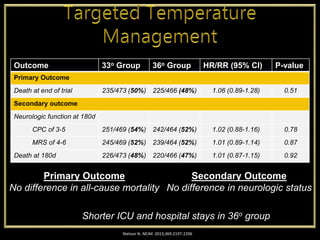
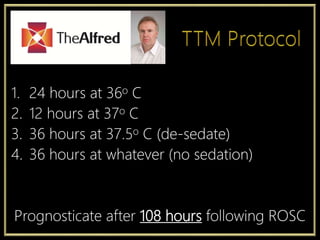
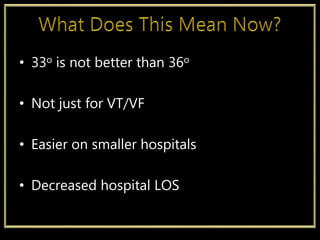
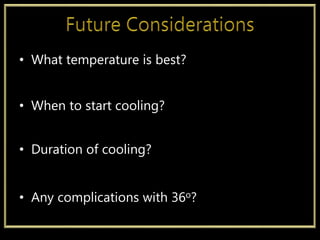
This document discusses the history and current state of therapeutic hypothermia after cardiac arrest. It begins with descriptions of early uses of cooling dating back to Hippocrates. Landmark studies from the 1960s-1980s helped establish the benefits of mild hypothermia (32-34°C) for neuroprotection. The 2002 HACA and Bernard trials showed improved outcomes with 24 hours of cooling. The 2013 Target Temperature Management trial found no additional benefit to cooling to 33°C versus 36°C for unshockable rhythms. It recommends a protocol of cooling for 24 hours at 36°C followed by rewarming over days and normal temperature by 108 hours. Ongoing questions remain around optimal temperature targets and duration.