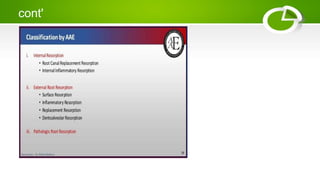
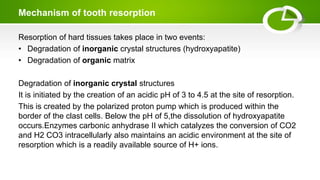
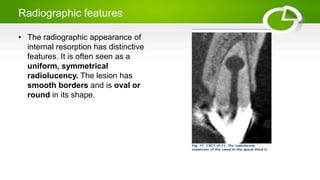
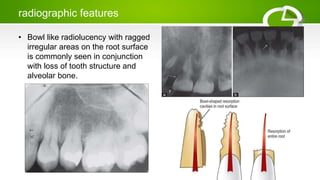
Tooth resorption can occur internally or externally and is classified based on location and etiology. Internal resorption is caused by damage to the pulp and occurs from within the tooth, appearing radiographically as a smooth, rounded radiolucency within the root canal. External resorption involves loss of cementum and dentin from outside the tooth, and appears as ragged radiolucencies on the root surface, often with accompanying bone loss. Management depends on severity and location of resorption and may include root canal therapy, surgery, or extraction.