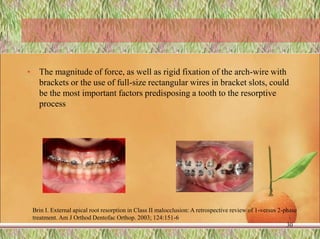
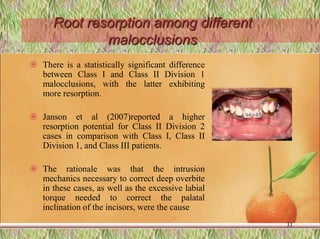
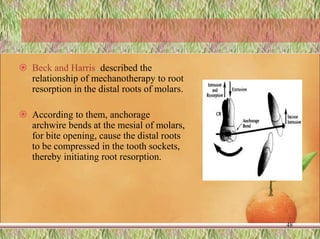
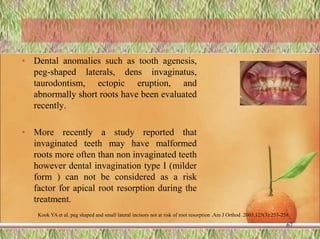
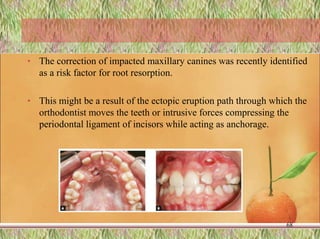
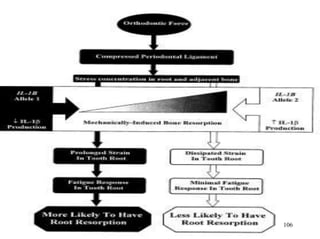
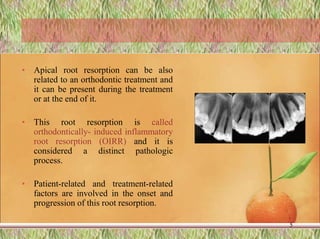
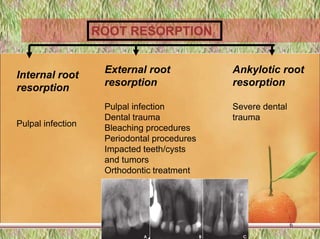
The document discusses root resorption, a condition involving the loss of root cementum and dentin, distinguishing between physiological resorption in deciduous teeth and pathological resorption in permanents, often exacerbated by orthodontic treatment. It outlines the classification, mechanisms, factors affecting root resorption, and emphasizes that both patient-related and treatment-related factors influence the severity and occurrence of this condition. The document concludes with the observation that while orthodontic forces can lead to root resorption, proper management and understanding of biological responses can aid in minimizing this iatrogenic effect.
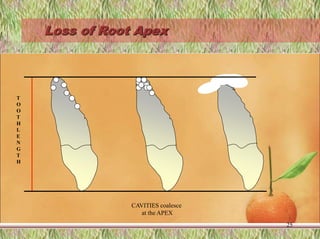
![Predisposing Patient [Biologic] Factors
› Individual susceptibility
› Genetics
› Systemic factors
› Nutrition
› Gender of the patient
› Chronologic age
› Dental age
› Tooth structure
› Traumatized teeth
› Presence of root resorption before orthodontic treatment
› Endodontically treated teeth
› Adverse habits as nail-biting, tongue thrusting
› Specific tooth vulnerability to tooth resorption
27](https://image.slidesharecdn.com/rootresorptionfinal-220610194150-ee809a9b/85/ROOT-RESORPTION-IN-ORTHODONTICS-27-320.jpg)
![• Treatment Related [Mechanical] Factors
– Type of orthodontic appliances used
– Magnitude of applied forces
– Direction of tooth movement
– Amount of tooth movement
– Jiggling and Occlusal trauma
• Combined Factors
– Treatment duration
– Root resorption detected radiographically during orthodontic
treatment
– Root resorption after appliance removal
– Relapse
28](https://image.slidesharecdn.com/rootresorptionfinal-220610194150-ee809a9b/85/ROOT-RESORPTION-IN-ORTHODONTICS-28-320.jpg)