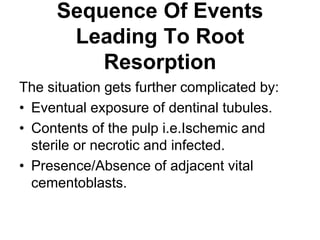
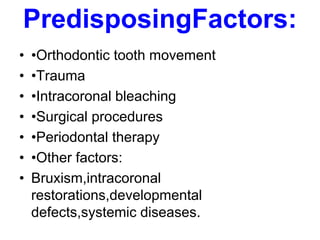
This document discusses different types of root resorption, including internal, external, inflammatory, and replacement resorption. It provides details on the definition, causes, mechanisms, diagnostic methods and treatment approaches for each type. The key types discussed are internal infection-related resorption, where necrotic infected pulp tissue triggers the resorption process, and external cervical resorption, which is often linked to trauma, restorations or orthodontic treatment. Diagnosis involves radiographs and vitality testing, while treatment focuses on removing resorptive tissue, root canal therapy if needed, and restoration.