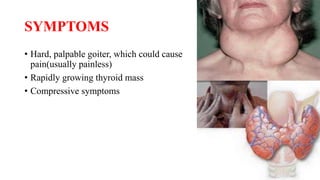
Riedel's thyroiditis is a rare form of thyroiditis characterized by the replacement of normal thyroid tissue with dense fibrosis that invades the surrounding structures of the neck. It is caused by an inflammatory process that infiltrates muscles and causes compressive symptoms. Diagnosis involves ruling out other types of thyroiditis through thyroid antibody tests and often biopsy. Treatment focuses on resection for severe compressive symptoms and use of tamoxifen, methotrexate, steroids, and thyroid hormone replacement for hypothyroidism. It is important to properly diagnose this rare condition to determine the appropriate treatment.