The document summarizes the key aspects of thyroid hormone synthesis and regulation. It discusses:
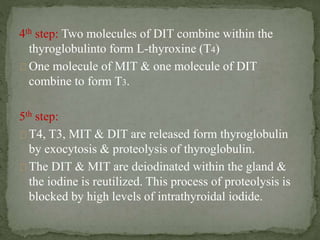
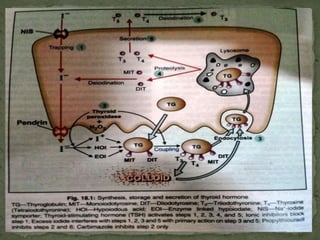
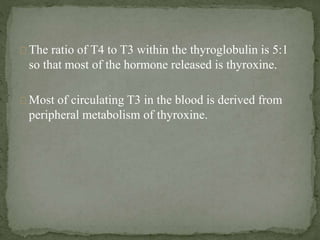
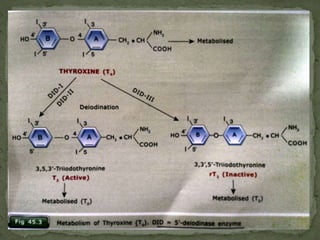
1) The thyroid gland secretes the hormones triiodothyronine (T3), tetraiodothyronine (T4), and calcitonin. T3 and T4 are synthesized from tyrosine residues within the thyroglobulin molecule through iodination and coupling reactions.
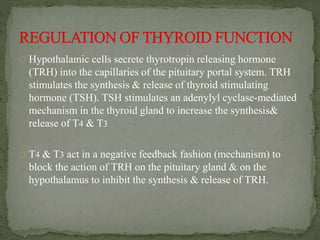
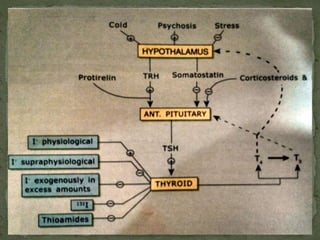
2) Thyroid stimulating hormone (TSH) from the pituitary stimulates thyroid hormone production and release, forming a negative feedback loop with T3 and T4.
3) Thyroid hormones regulate growth, development, metabolism and have wide-ranging effects in the body through nuclear receptors that control gene expression.