1. The thyroid gland secretes thyroid hormones that regulate metabolism and growth. Thyroid hormones are synthesized within thyroid follicles by iodination of tyrosine residues on thyroglobulin.
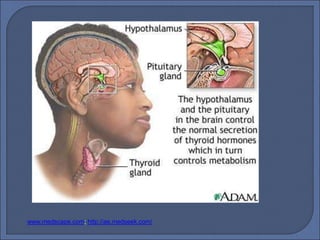
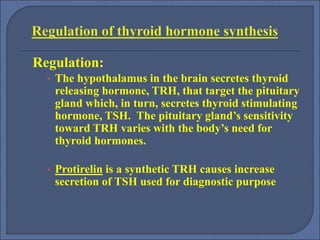
2. Thyroid hormone synthesis and secretion is regulated by a negative feedback loop involving thyroid stimulating hormone (TSH) from the pituitary gland.
3. Disorders of the thyroid gland include hyperthyroidism (overproduction of hormones) and hypothyroidism (underproduction of hormones).