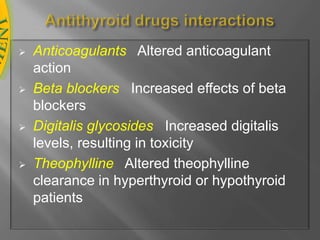
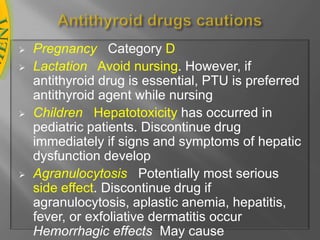
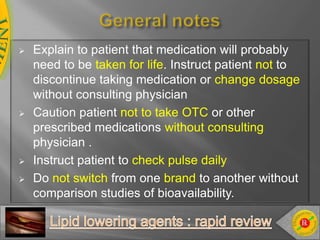
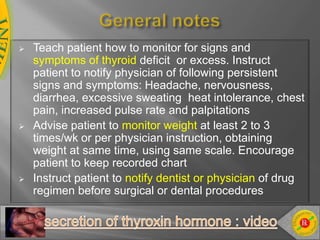
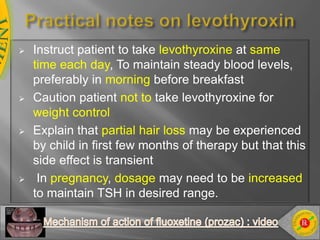
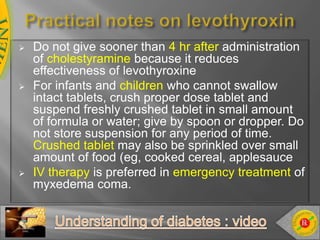
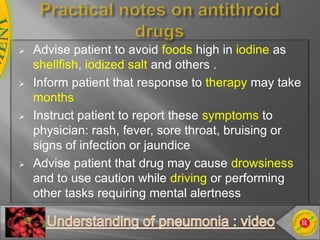
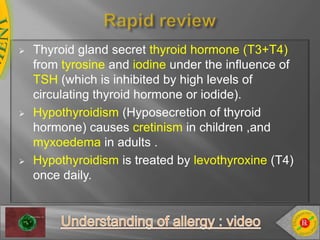
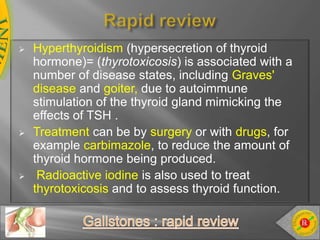
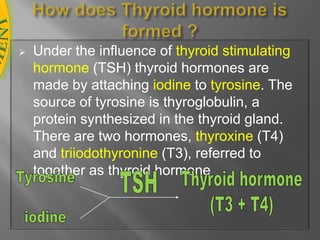
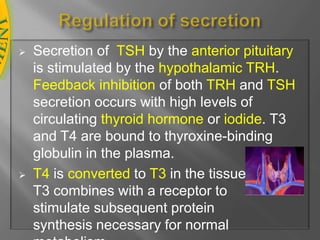
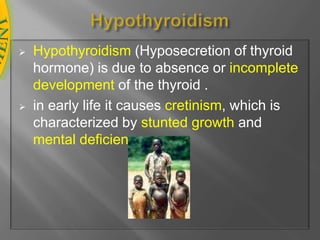
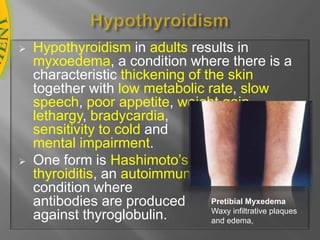
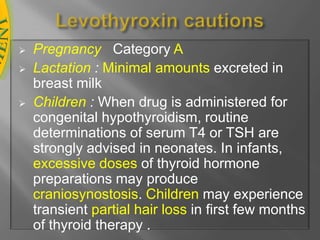
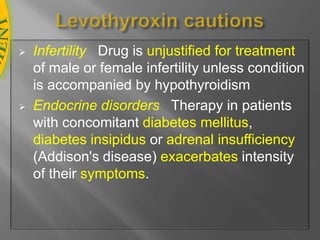
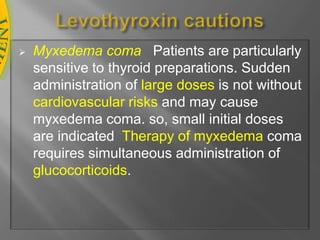
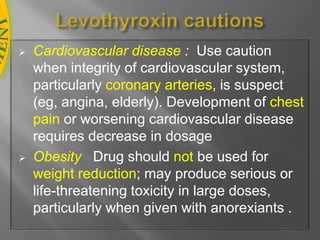
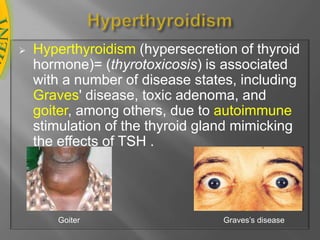
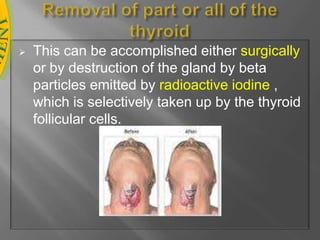
This document discusses thyroid hormone disorders, including hypothyroidism and hyperthyroidism, detailing the thyroid gland's function, hormone production, and the implications of each disorder. Hypothyroidism is characterized by low hormone levels leading to conditions like cretinism and myxedema, whereas hyperthyroidism involves excess hormone secretion from diseases such as Graves' disease. Treatment options for both conditions include hormone replacement therapy with levothyroxine and antithyroid medications, with important cautions regarding their use in different populations.


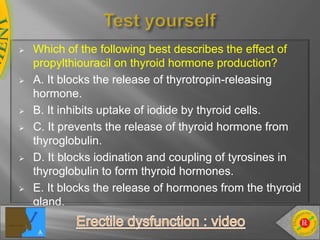
![The effects of these drugs are slow in onset and thus they are not effective in the treatment of thyroid storm.Additive drugsPropranolol: beta-Blockers are effective in blunting the widespread sympathetic stimulation that occurs in hyperthyroidism .Mechanism of action of antithyroidPropylthiouracil and carbimazole are concentrated in the thyroid where they inhibit the iodination of tyrosyl groups and the coupling of iodotyrosines to form T3 and T4 . PTU can also block the conversion of T4 to T3. [Note: These drugs have no effect on the thyroglobulin already stored in the gland; therefore observation of any clinical effect of these drugs may be delayed until thyroglobulin stores are depleted.] Administration of antithyroid drugsPropylthiourathil (PTU) is given each 8 hr (to maintain serum drug levels) whereas a single dose of carbimazole is sufficient due to the long duration of its antithyroid effect.](https://image.slidesharecdn.com/thyroidglanddisorders-100816080143-phpapp02/85/Thyroid-gland-disorders-27-320.jpg)