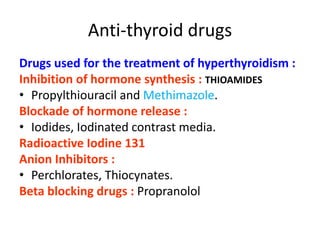
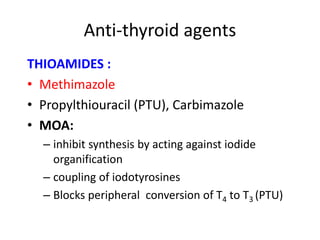
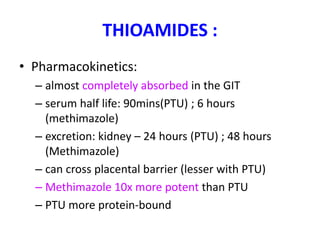
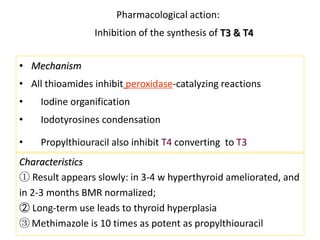
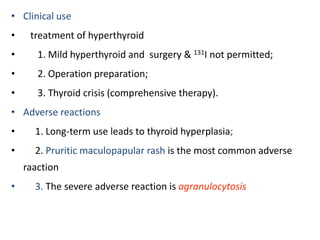
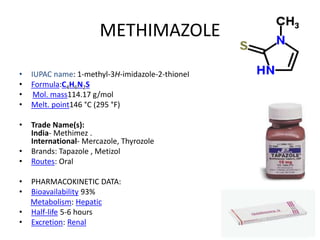
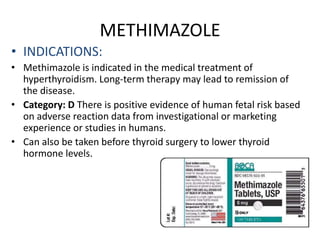
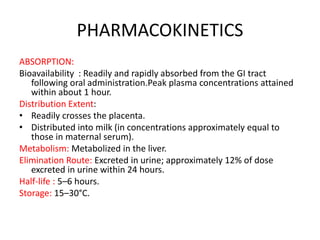
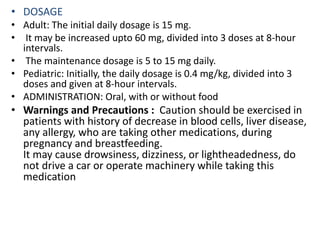
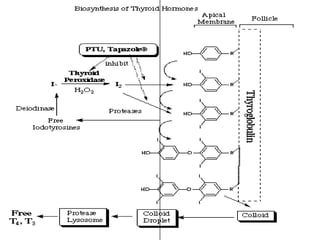
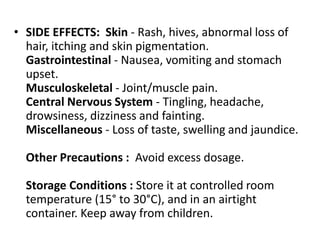
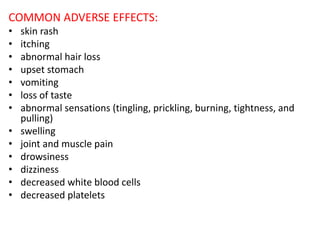
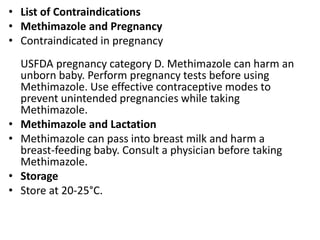
Methimazole is an oral antithyroid drug used to treat hyperthyroidism. It works by inhibiting the synthesis of thyroid hormones in the thyroid gland. Common side effects include skin rash, upset stomach, and loss of taste. Methimazole is readily absorbed from the gastrointestinal tract and metabolized in the liver. It has a half-life of 5-6 hours and is excreted in urine. Due to risks of harming an unborn baby, methimazole is contraindicated in pregnancy and breastfeeding without physician consultation.