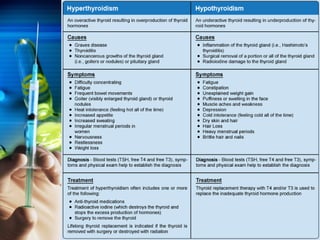
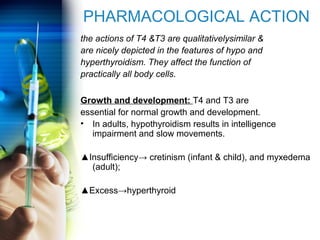
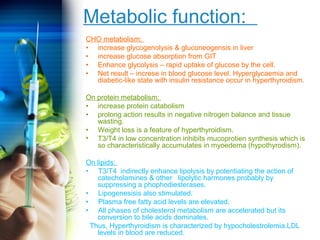
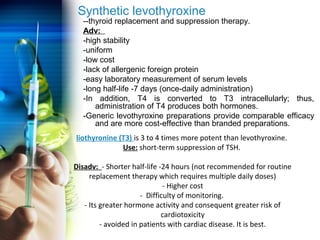
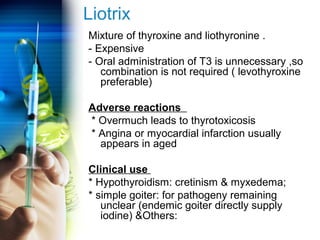
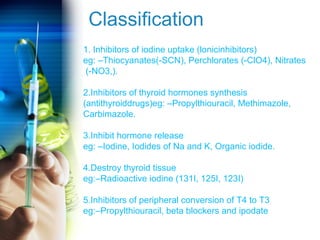
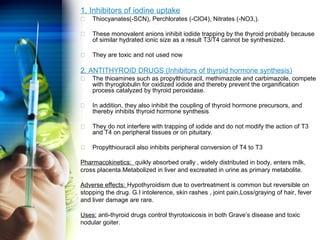
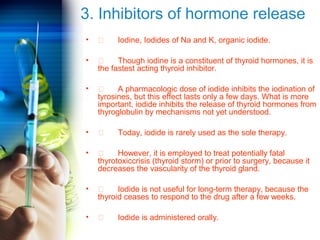
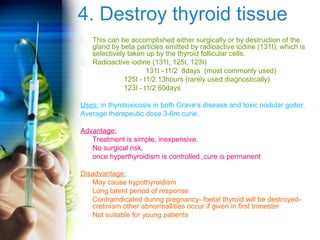
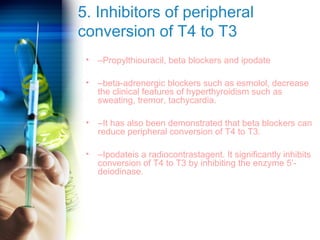
The document discusses thyroid and antithyroid drugs, covering the synthesis, transport, and mechanisms of thyroid hormones (T3 and T4), as well as their physiological effects and roles in various diseases. It details the actions of these hormones on metabolism, growth, and the nervous system, as well as pharmacotherapeutic approaches to treat conditions like hypothyroidism and hyperthyroidism. Additionally, it outlines various treatment options, their mechanisms, pharmacokinetics, and potential adverse reactions.