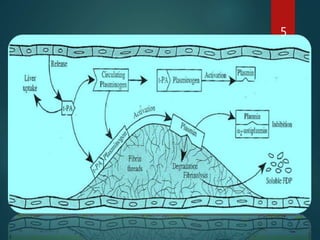
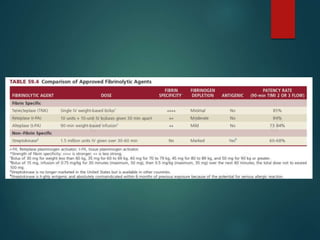
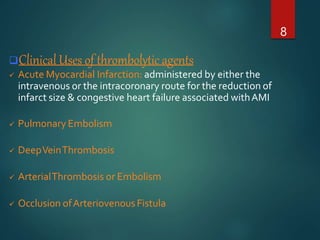
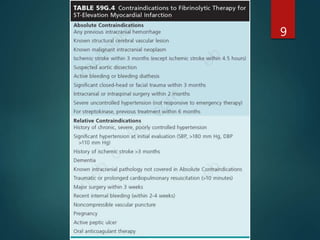
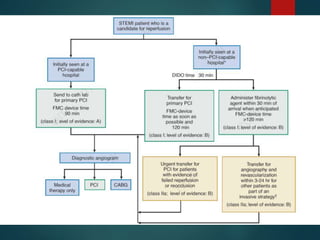
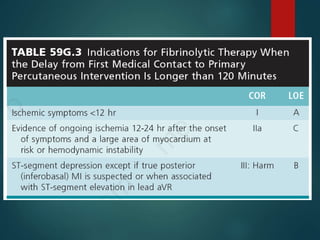
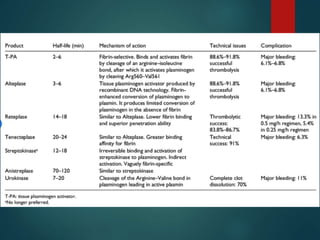
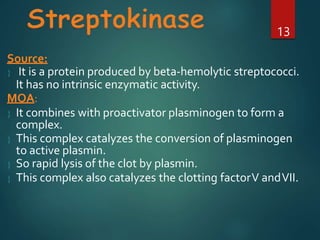
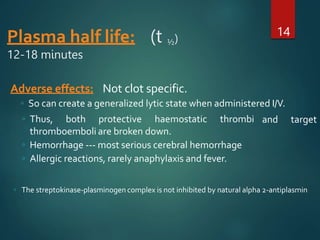
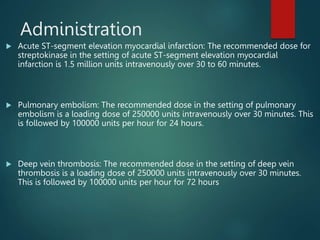
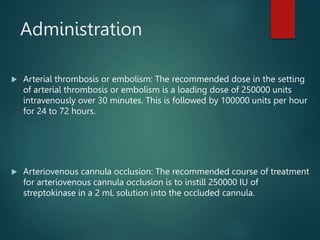
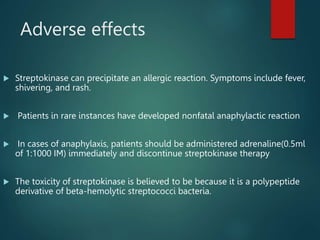
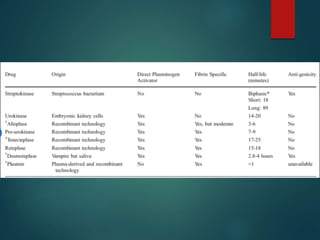
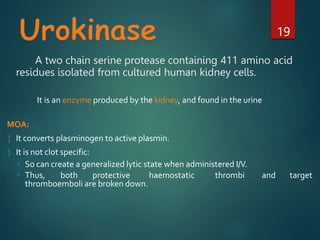
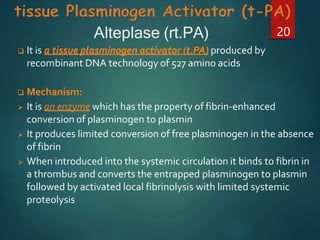
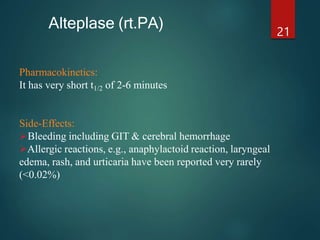
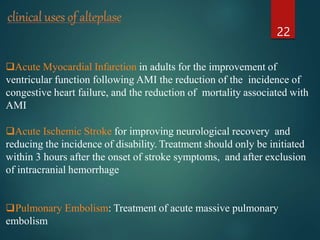
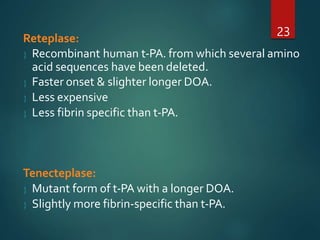
Thrombolytic agents work by activating plasminogen to form plasmin, which breaks down fibrin in blood clots. The document discusses several thrombolytic agents: streptokinase works by forming a complex with plasminogen to catalyze its activation; alteplase is a recombinant tissue plasminogen activator that selectively activates plasminogen bound to fibrin clots; and reteplase and tenecteplase are modified forms of tPA with longer durations of action. Thrombolytic agents are used to treat conditions caused by blood clots such as myocardial infarction, pulmonary embolism, and ischemic stroke.