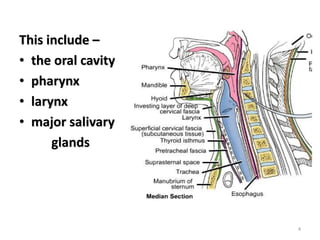
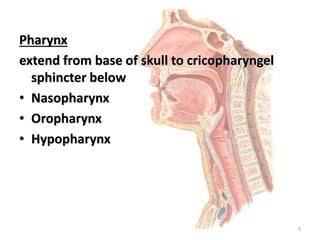
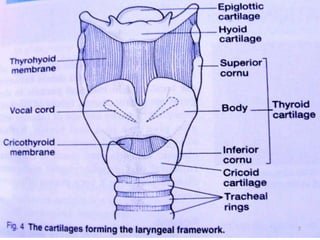
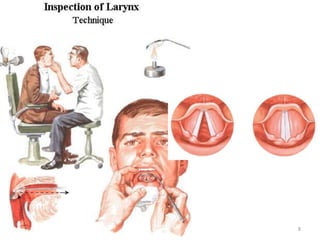
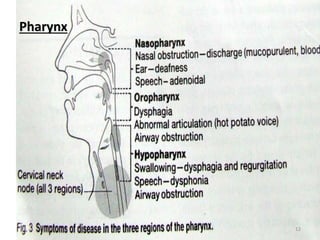
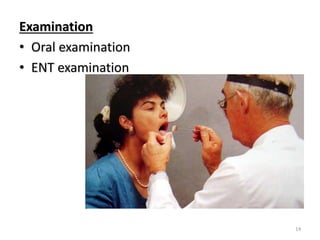
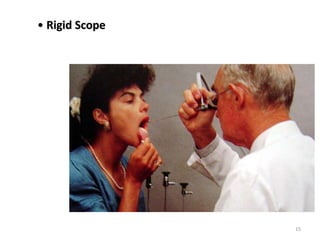
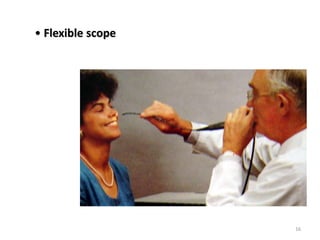
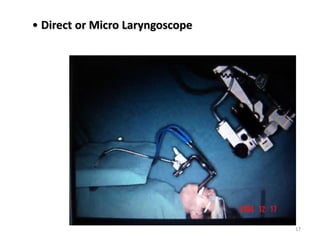
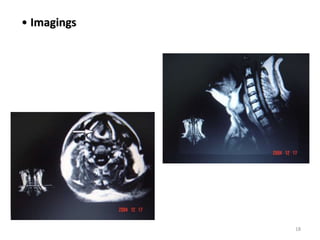
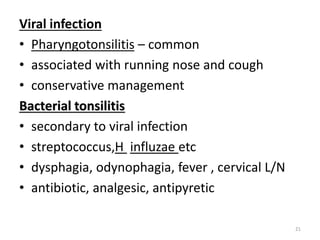
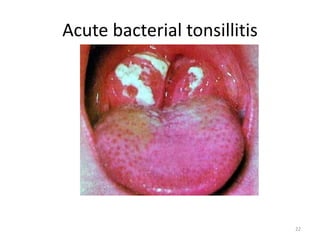
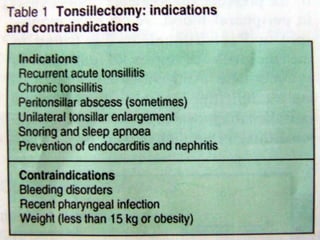
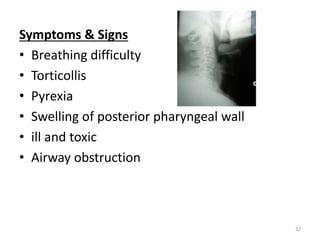
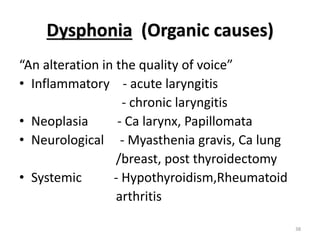
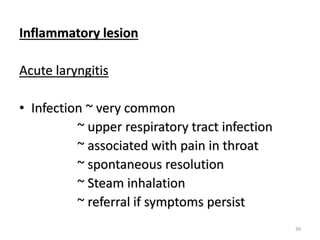
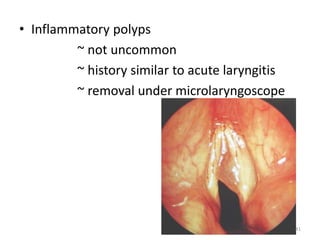
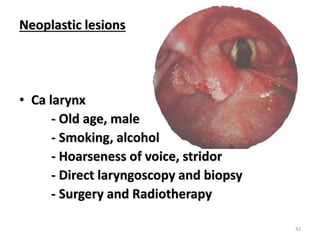
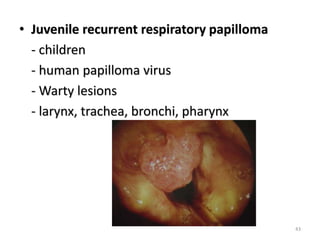
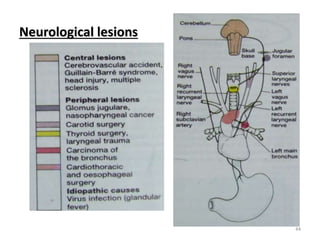
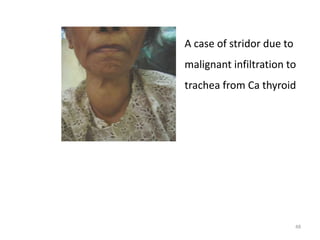
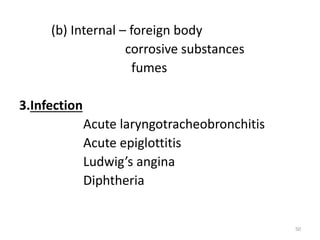
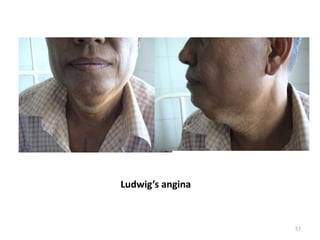
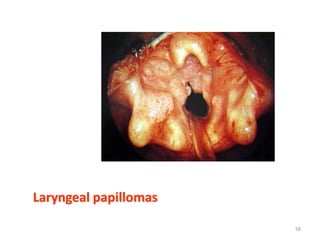
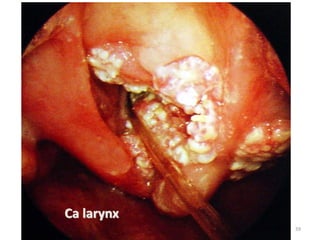
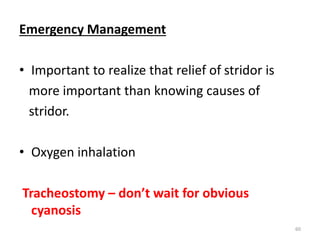
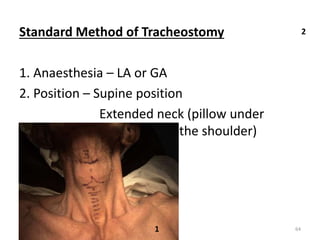
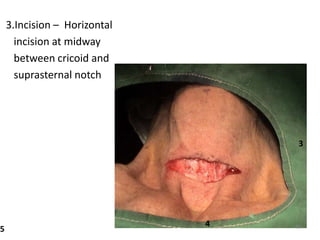
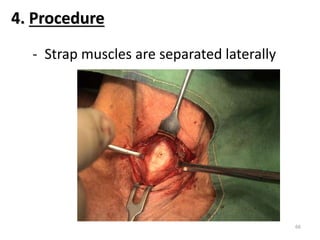
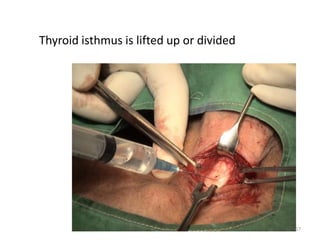
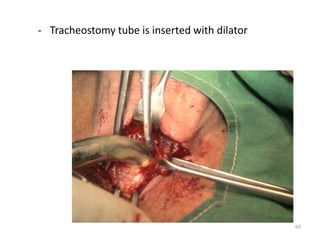
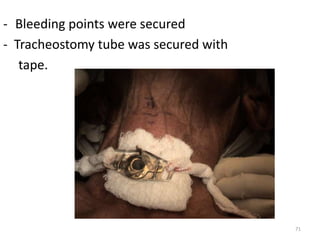
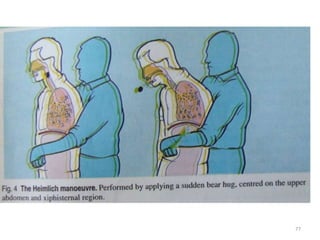
This document provides information about anatomy and functions of the throat (oral cavity, pharynx, larynx, salivary glands), as well as common symptoms, signs, and conditions that can affect the throat, including sore throat, abscesses, dysphonia, and stridor. It discusses the causes, symptoms, signs, and management of various throat conditions like peritonsillar abscess, Ludwig's angina, retropharyngeal abscess, parapharyngeal abscess, laryngitis, papillomas, and cancer of the larynx. Tracheostomy indications and techniques are also summarized.