This document summarizes research on thiamine (vitamin B1) deficiency, with a special focus on infantile (beriberi) form. It discusses:
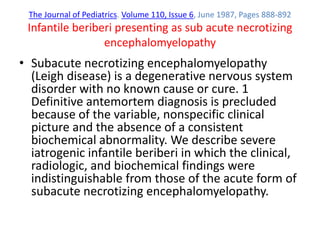
1) Thiamine's role as a coenzyme in energy production and its deficiency leading to energy deprivation in high-energy organs like brain, heart and nerves.
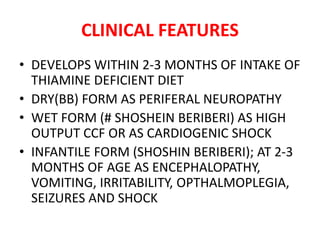
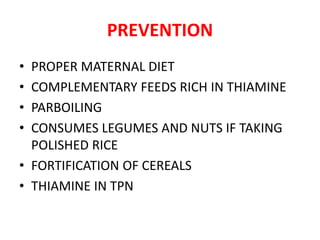
2) Risk factors for deficiency including alcoholism, polished rice diets, pregnancy, critical illness, and refugees. Deficiency develops within 2-3 months and causes encephalopathy, vomiting and irritability in infants.
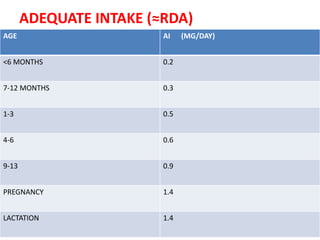
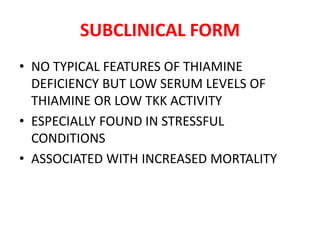
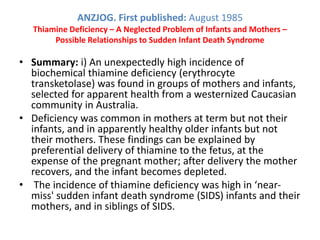
3) Several studies finding unexpectedly high rates of subclinical and clinical thiamine deficiency in infants and mothers in various countries, linked to polished

![American Journal of Clinical Nutrition 1966 Vol.18 No.4 pp.275-7
Childhood Thiamine Deficiency in Northern Thailand.
• 45 children suspected of having beriberi were
admitted, 91% were under the age of 1 year, with a
peak in incidence between 1 and 3 months
• In Thailand a high mortality occurs in infants in the
second month of life and a correlation between the
mortality and thiamine deficiency is suggested. Similar
trends in mortality associated with infantile beriberi
have been recorded in India [this Bulletin, 1942, v. 39,
330] and Vietnam (Tu, Contribution to the study of
infantile beriberi in Vietnam, Saigon. Thesis, 1954,
Hanoi). W. R. Aykroyd.](https://image.slidesharecdn.com/thaimine-170331134943/85/Thaimine-12-320.jpg)
![PLOS. Published: February 22, 2011
Clinically Unapparent Infantile Thiamin Deficiency in Laos
• Overt infantile beriberi is relatively easy to diagnose but may
be the tip of a much larger iceberg of deficiency. A significant
proportion of infants admitted with other diseases, such as
acute respiratory infection or diarrhoea, may also have
clinically unapparent thiamin deficiency contributing to the
illness, and thiamin treatment may improve their outcome
• This study suggests that a substantial minority of infants
(13.4%) admitted without clinical evidence of beriberi had
biochemical thiamin deficiency.
• There is evidence that gastrointestinal absorption of thiamin
is saturated at doses of >5 mg [5], suggesting that oral doses
above this give limited, if any, benefit](https://image.slidesharecdn.com/thaimine-170331134943/85/Thaimine-19-320.jpg)