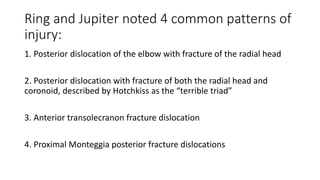
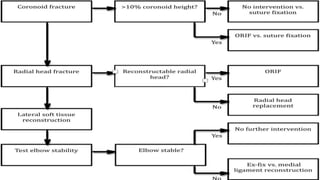
1. The document discusses fracture dislocations of the elbow, which are complex injuries that often require surgical intervention due to associated fractures.
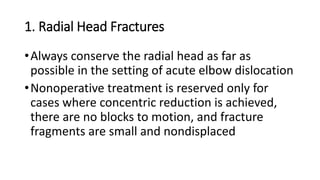
2. Common fracture patterns include posterior dislocations with radial head or coronoid fractures. Surgical fixation may involve screws, plates, or replacement of fractured bone.
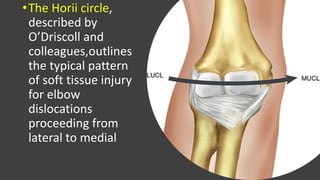
3. Soft tissue injuries like lateral collateral ligament avulsions must also be repaired to prevent recurrent instability.
4. Potential complications addressed include heterotopic ossification, recurrent instability, ulnar neuropathy, arthrofibrosis, and post-traumatic arthrosis. Careful restoration of bony and soft tissue anatomy can help reduce complications.


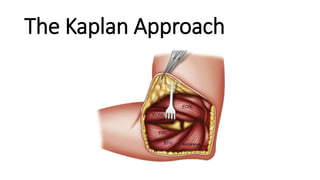
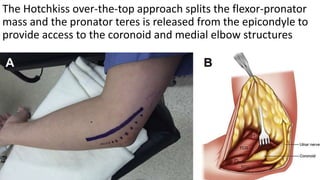
![•Medially, an anteromedial interval between the
pronator teres and brachialis may be used to
access the anterior capsule.
•The posteromedial (flexor carpi ulnaris [FCU]-
splitting) exposure necessitates anterior ulnar
nerve transposition and the FCU is divided
between the 2 heads of the muscle](https://image.slidesharecdn.com/200324complexelbowdislocations-200512073550/85/200324-Complex-elbow-dislocations-19-320.jpg)