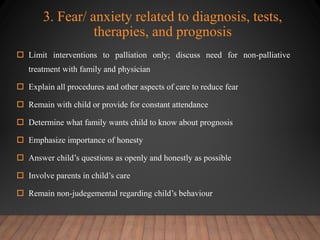
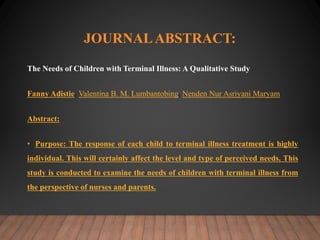
A terminal illness in a child is traumatic for the child and family as it destroys their life plans. A terminally ill child is one who will die soon from an incurable disease. Nursing care involves providing age-appropriate information to the child and family, managing symptoms, and supporting the emotional needs of all involved through the end of life. Decision making is a collaborative process that considers the child and family's needs and wishes. The goal is to ensure the child's comfort and allow them to live fully until death.