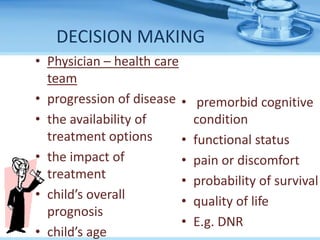
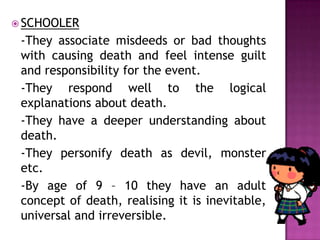
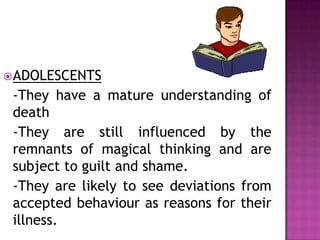
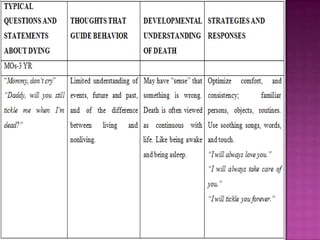
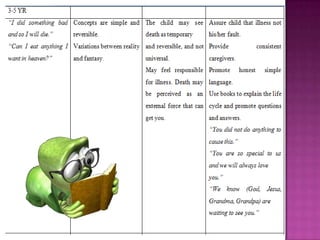
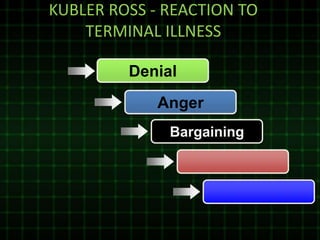
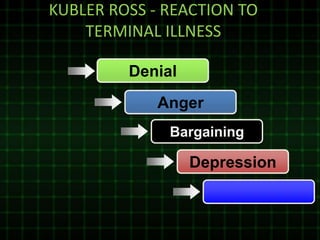
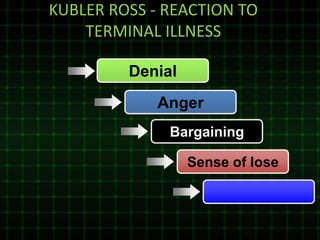
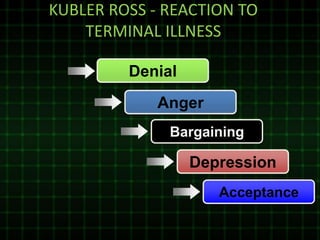
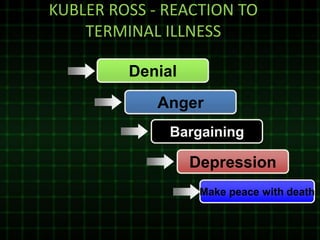
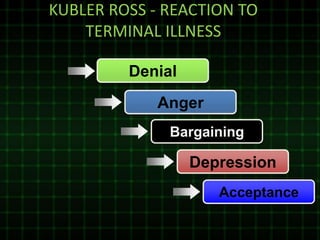
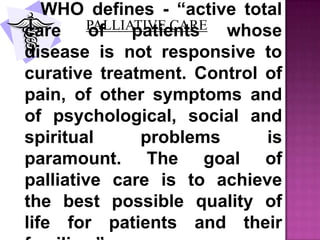
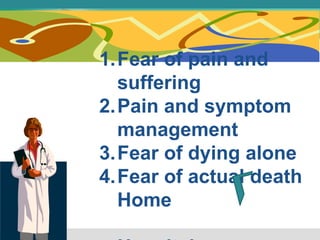
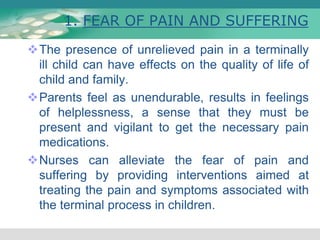
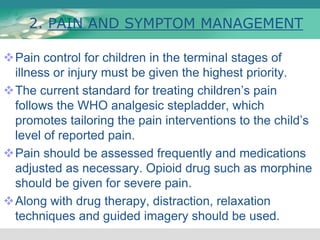
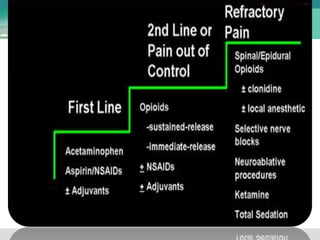
This document discusses terminal illness and death in children. It covers concepts like acute, chronic and terminal illnesses. A terminally ill child is defined as one who cannot be cured and is expected to die within a short time from their disease. When making decisions, factors like the child's prognosis, treatment options and quality of life are considered. Care can involve hospitals, home care or hospice care. Nursing management focuses on relieving pain, symptoms and fears while supporting the child and family.