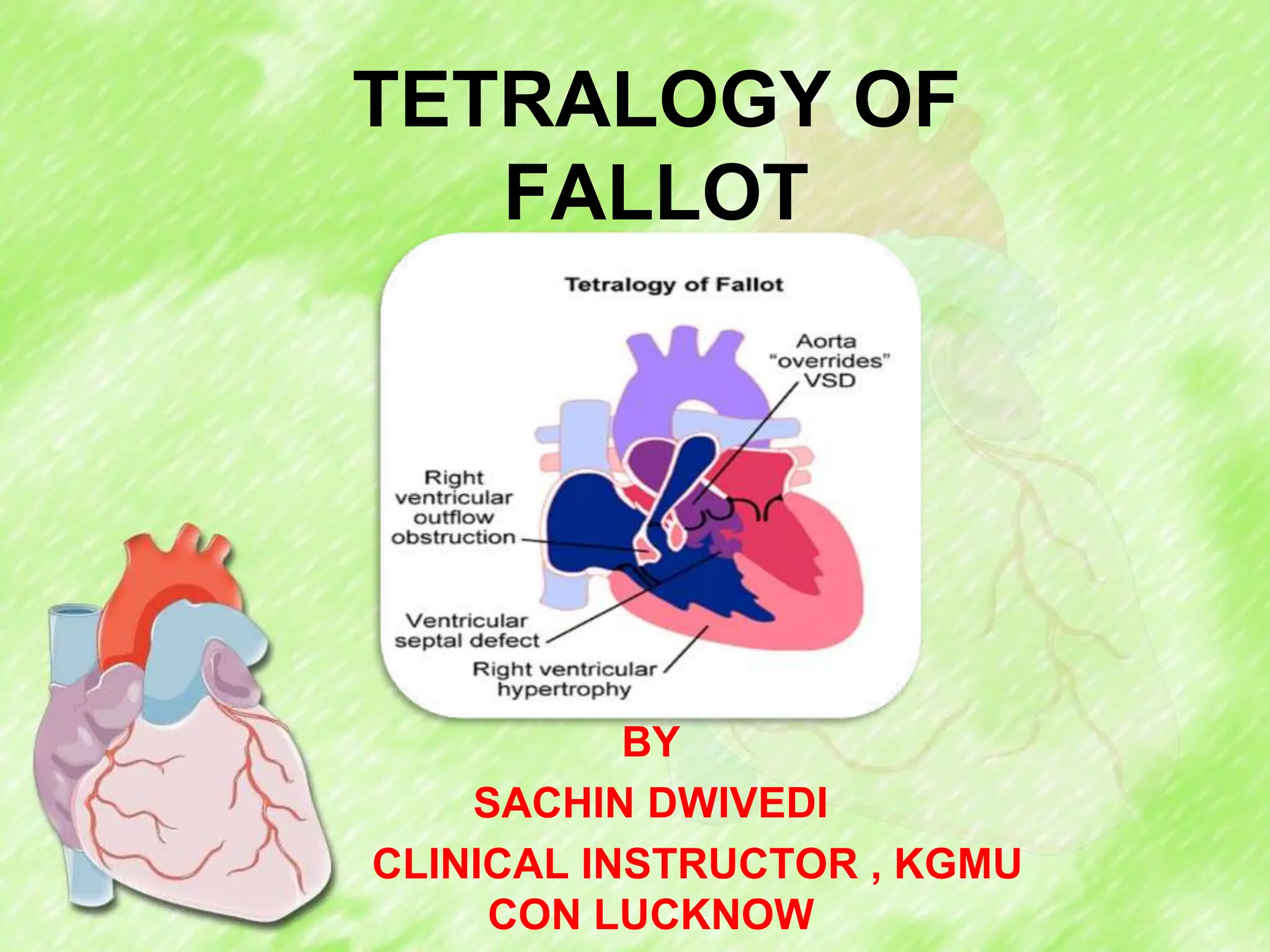
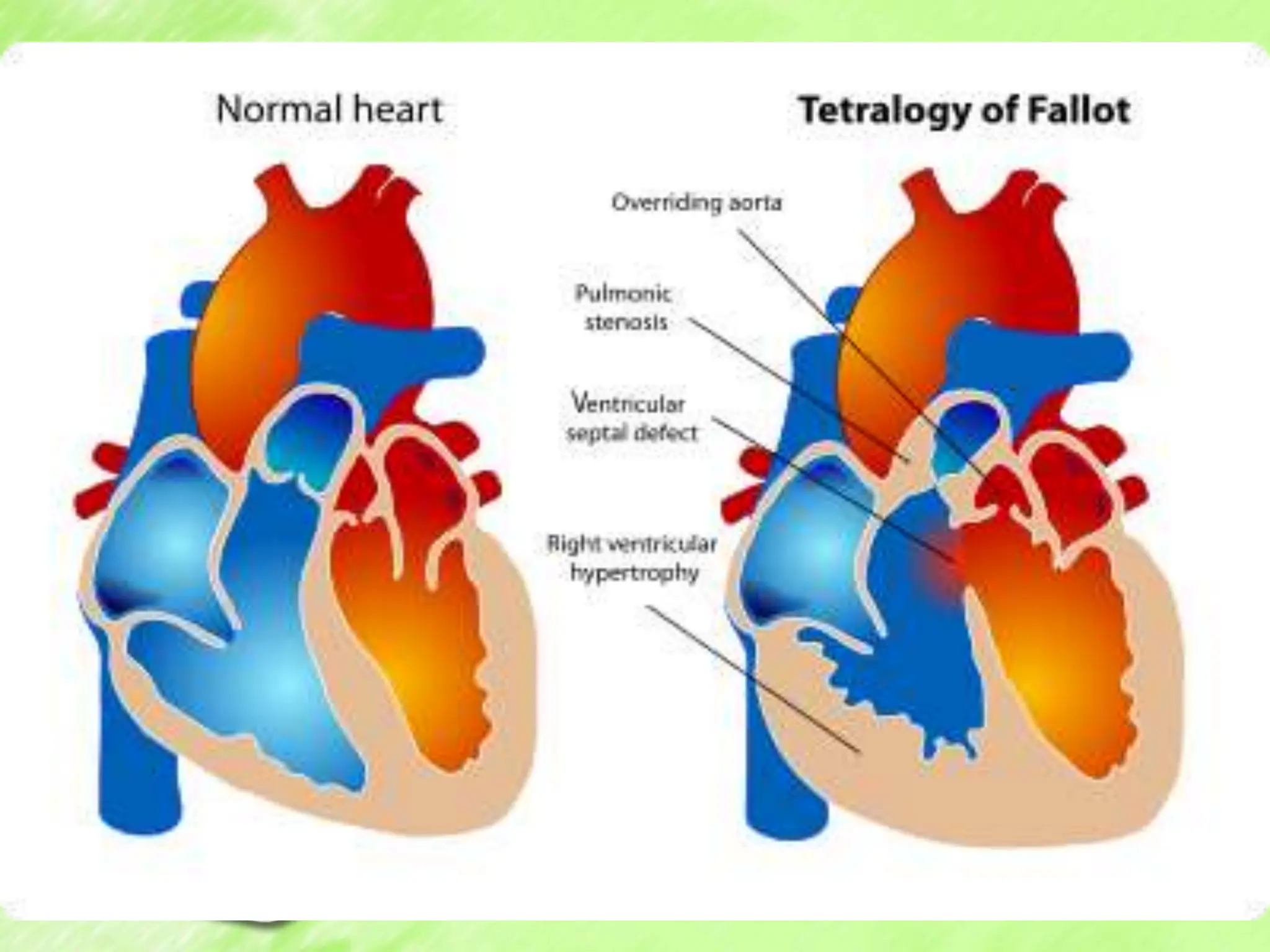
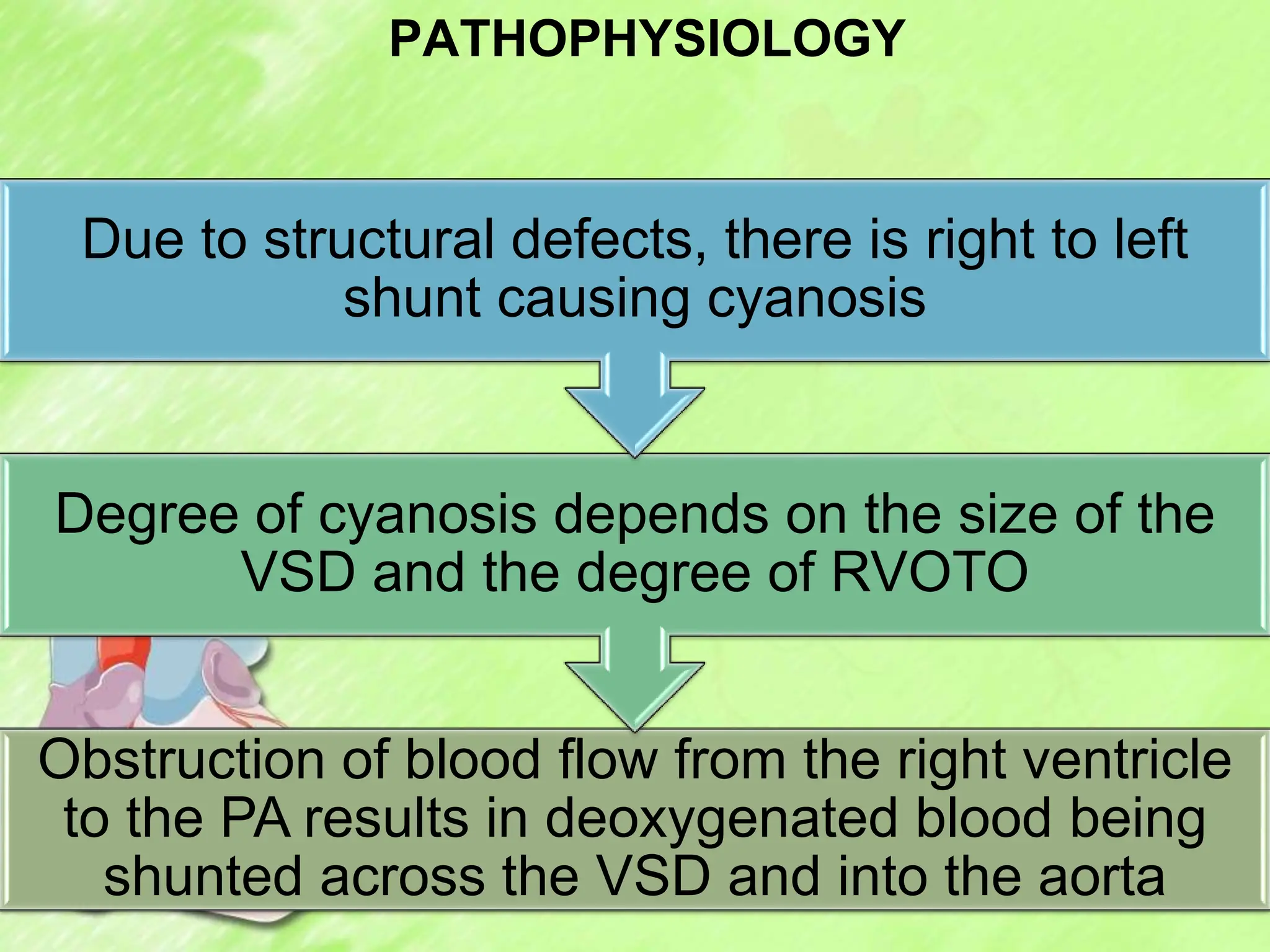
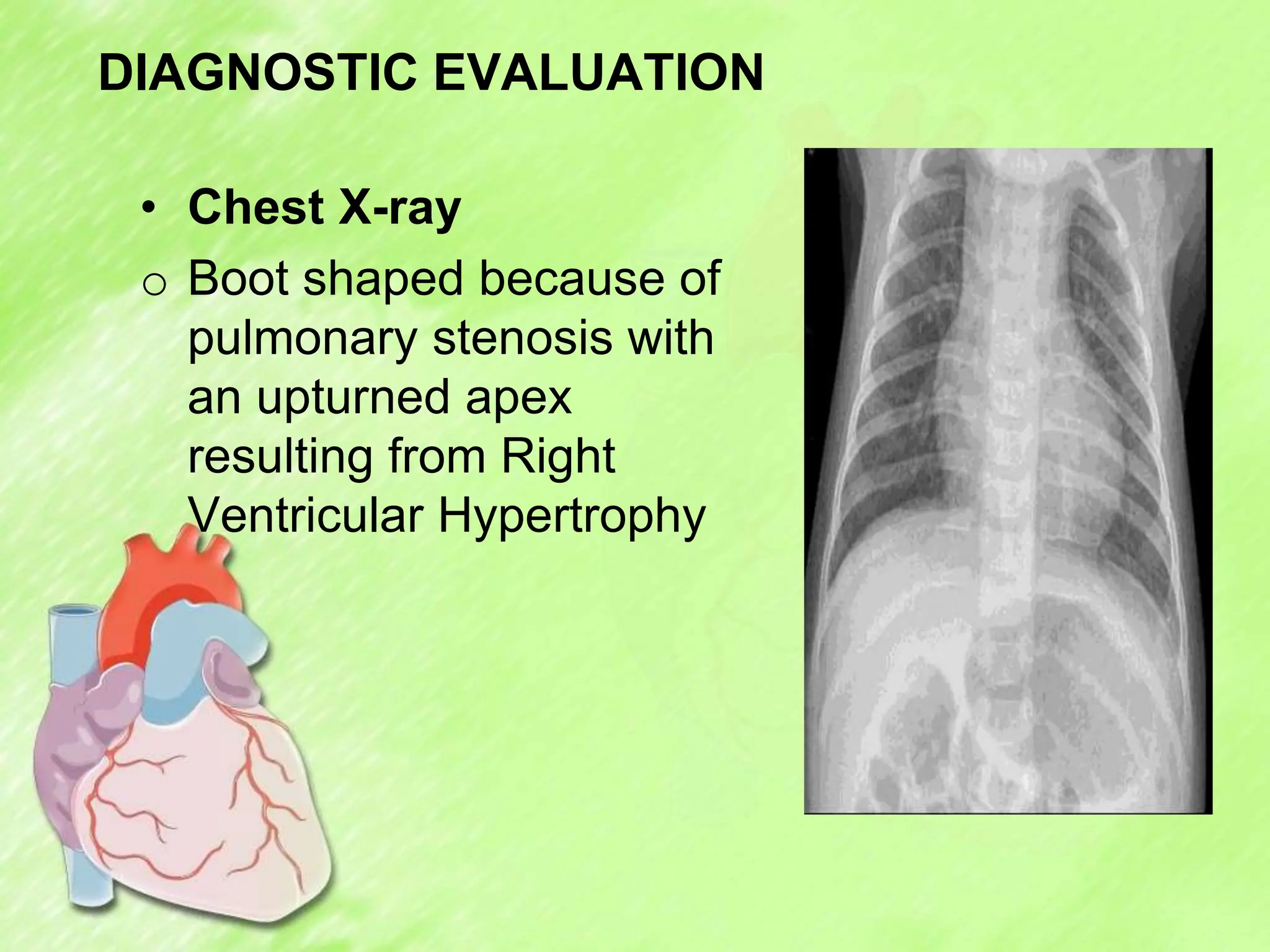
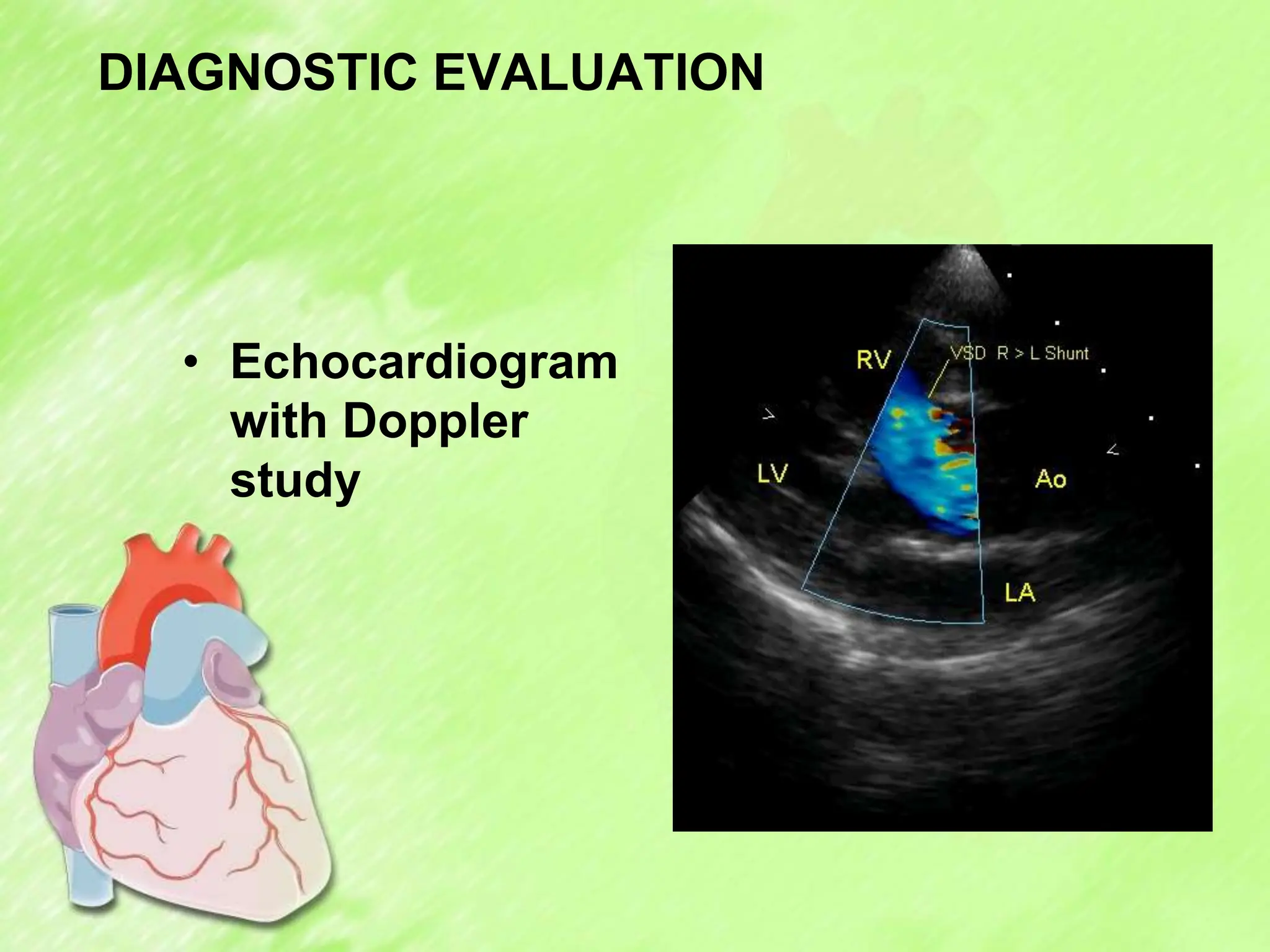
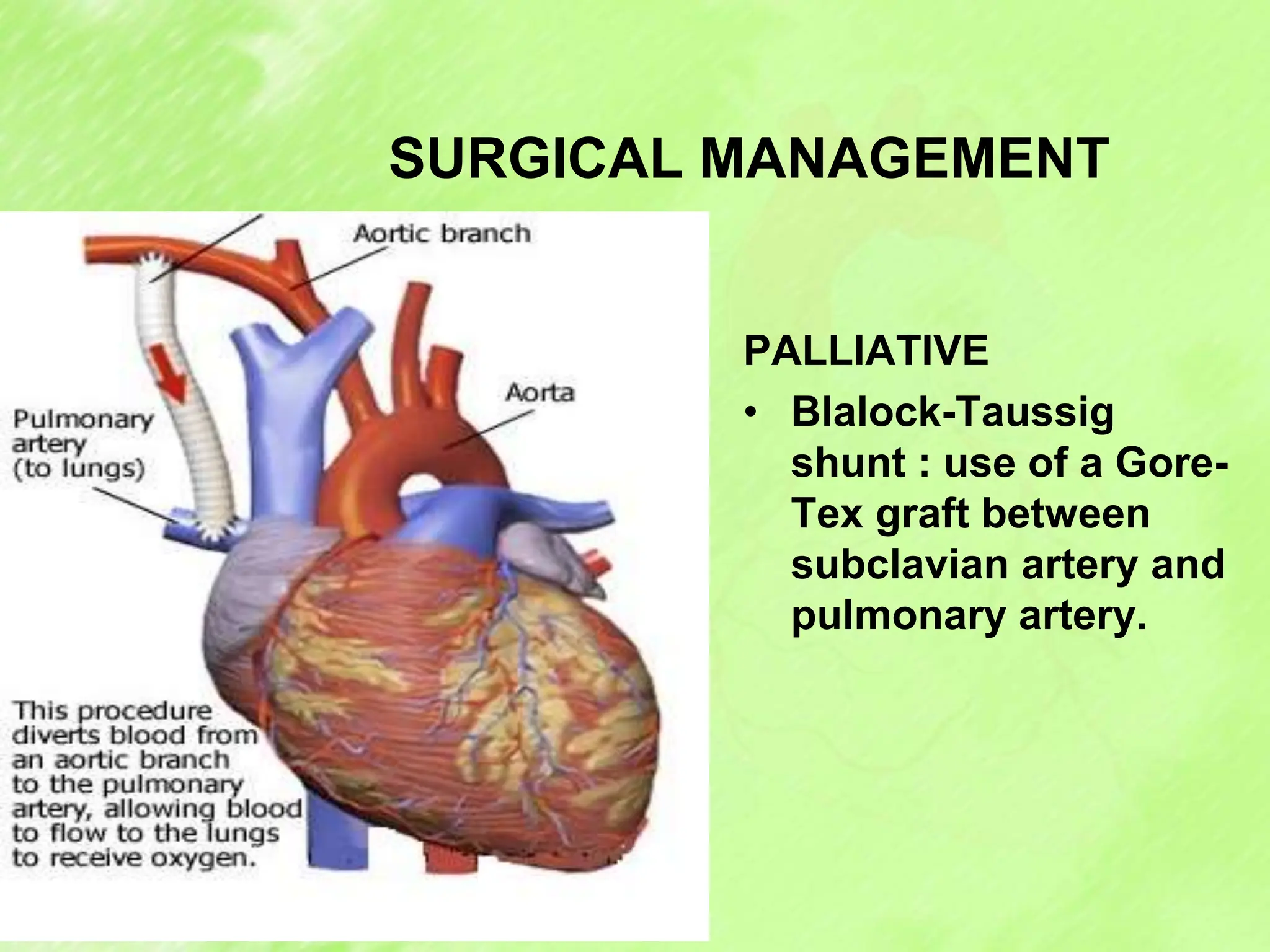
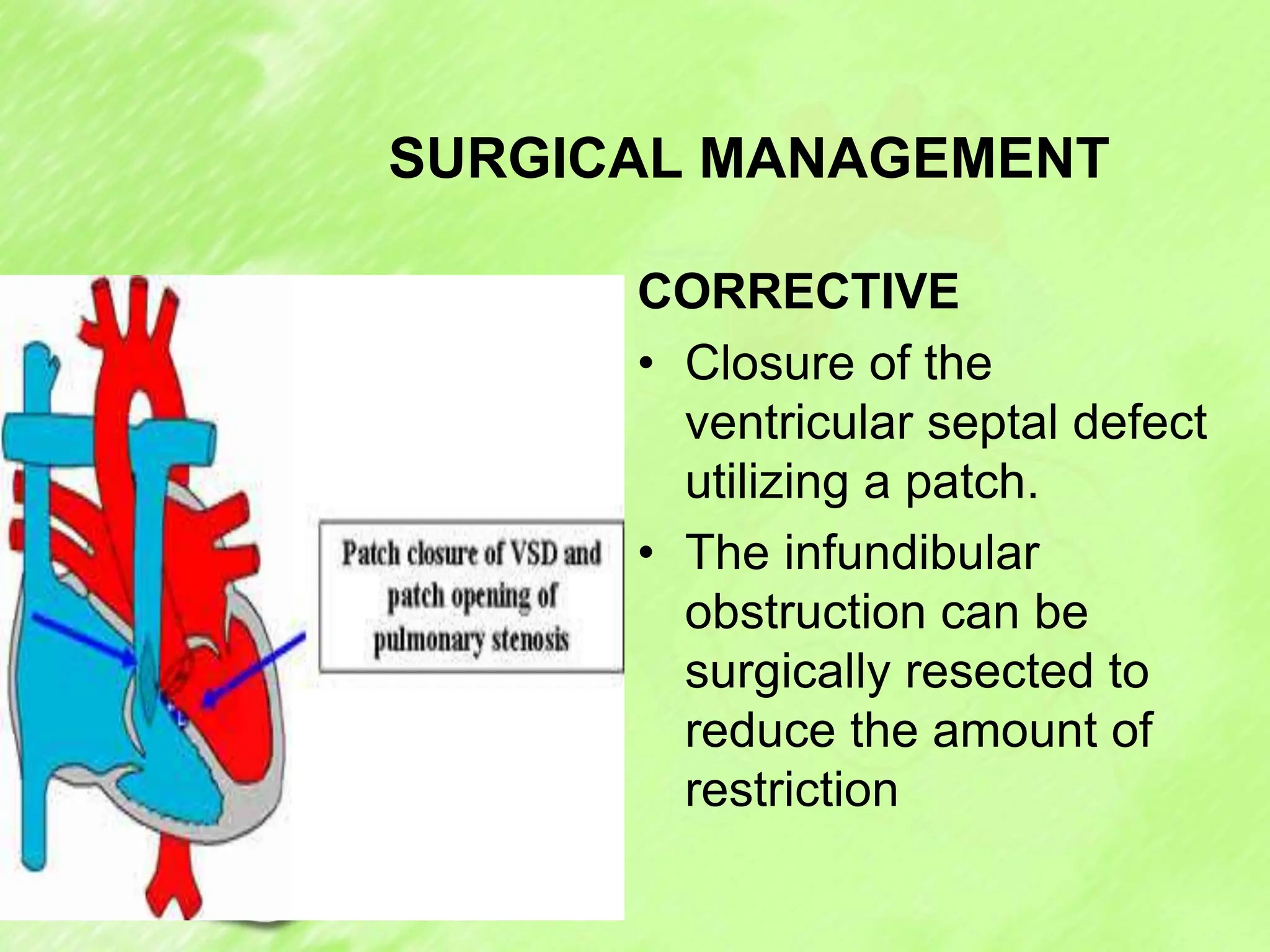
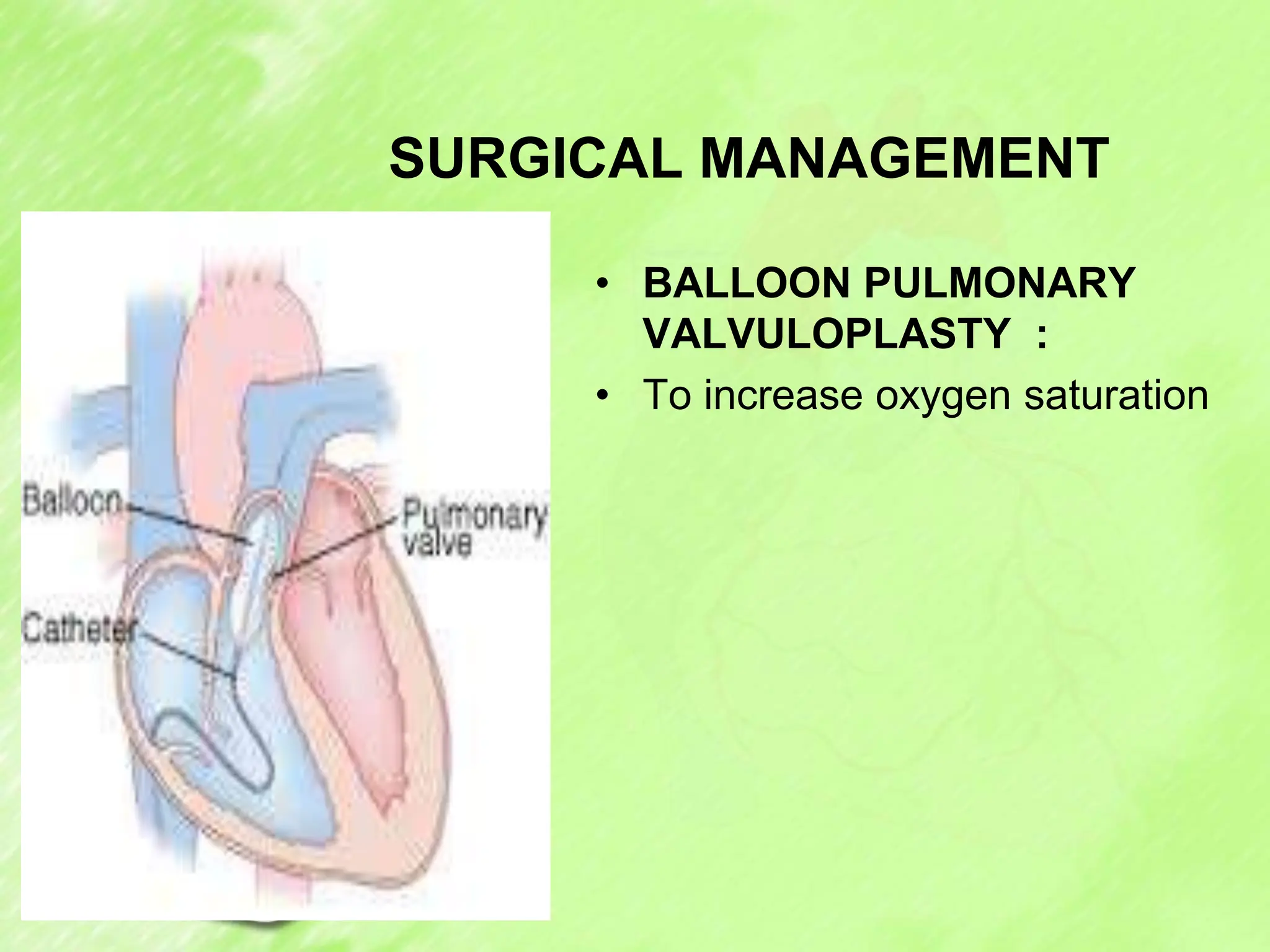
Tetralogy of Fallot (TOF) is the most common cyanotic congenital heart defect characterized by four abnormalities: pulmonary stenosis, ventricular septal defect, overriding aorta, and right ventricular hypertrophy. It results in deoxygenated blood being shunted to the body instead of the lungs. Clinical manifestations include cyanosis, clubbing, and decreased activity tolerance. Diagnosis involves echocardiogram, chest X-ray, and cardiac catheterization. Management includes supplemental oxygen, medications during spells, and complete surgical repair typically before age 2 to close defects and reduce obstructions. Complications can include hypoxia, heart failure, and arrhythmias if left untreated.