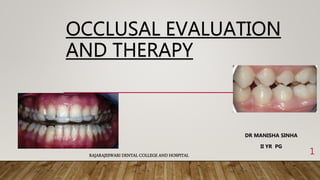
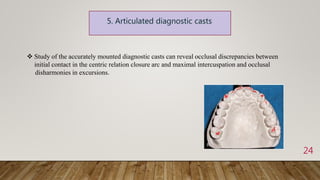
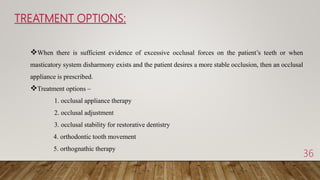
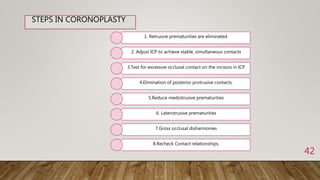
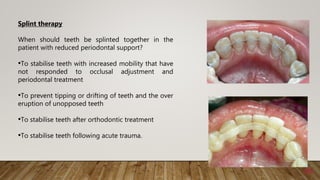
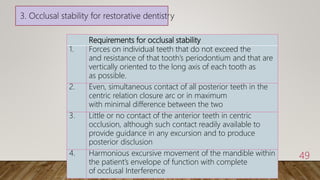
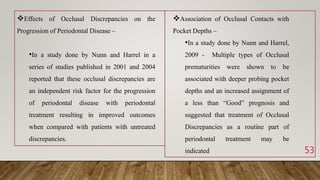
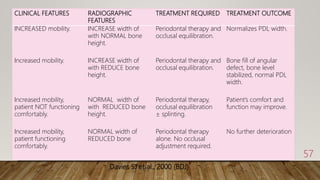
This document provides an overview of occlusion and occlusal therapy. It discusses the forces involved in jaw movement, the biologic basis of normal occlusion and occlusion-related dysfunction. It covers clinical examination techniques used to evaluate occlusion and various occlusal therapies including occlusal appliances, occlusal adjustment, splint therapy and orthodontic treatment. The goal of occlusal therapy is to establish stable functional relationships that are favorable for oral health by reducing excessive occlusal forces and correcting occlusal disharmonies.