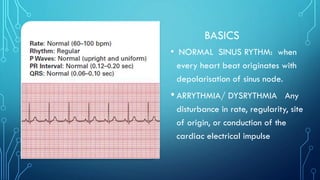
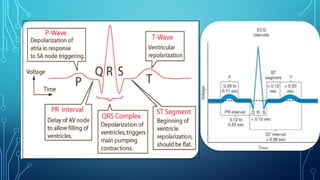
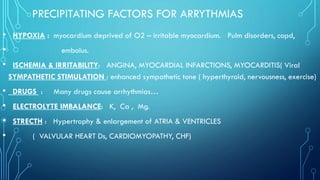
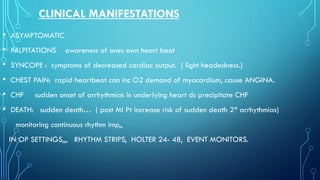
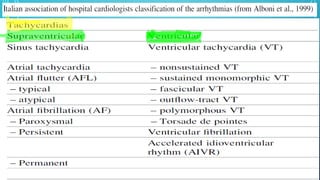
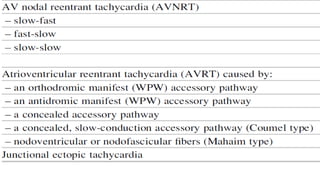
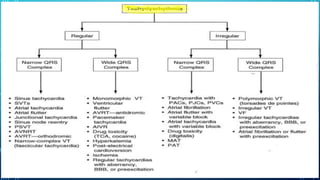
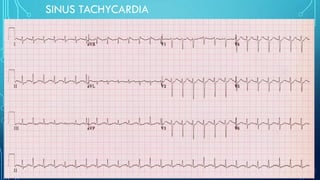
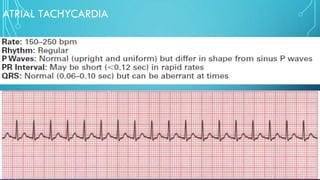
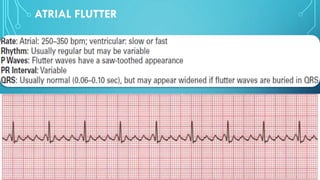
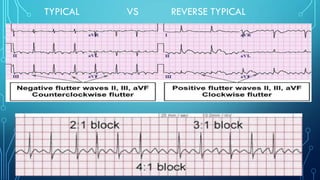
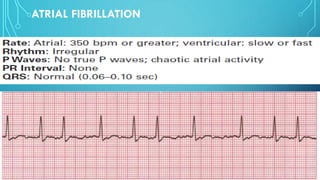
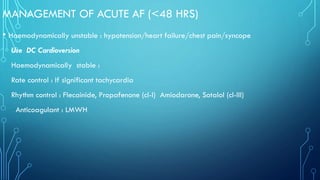
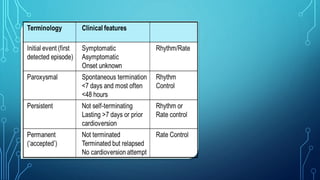
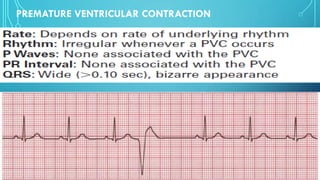
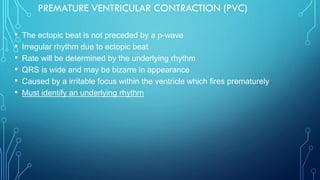
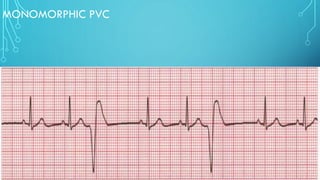
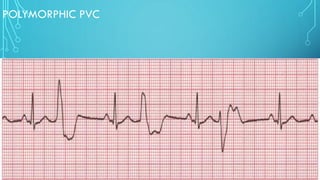
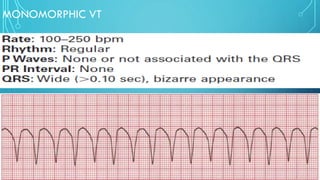
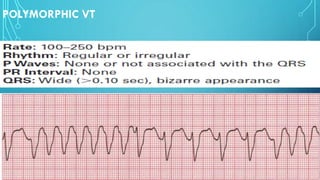
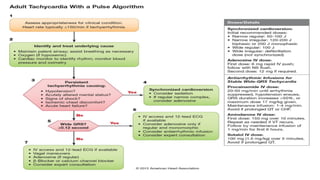
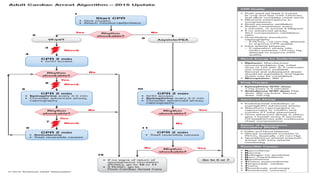
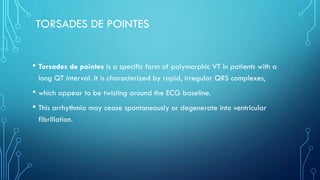
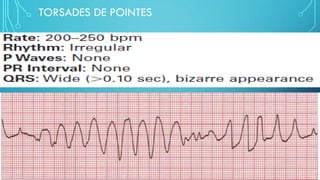
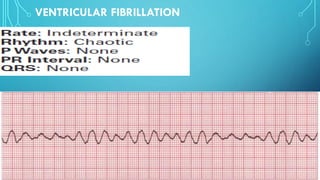
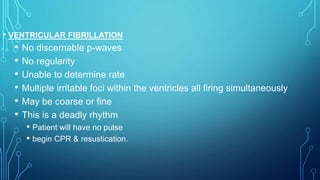
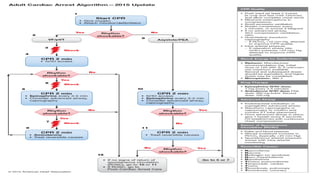
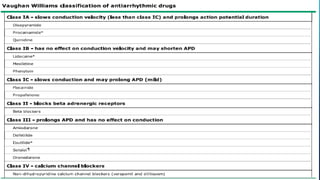
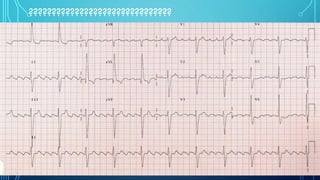
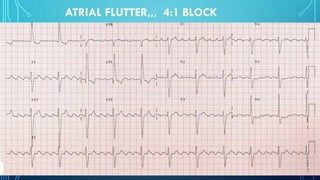
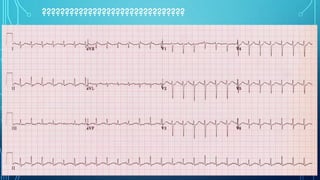
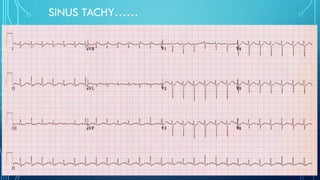
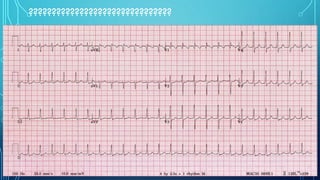
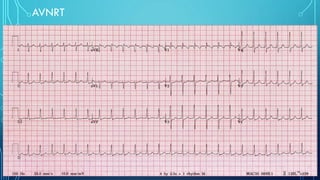
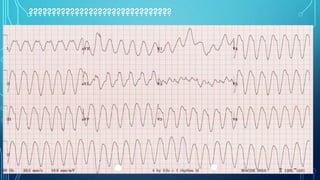
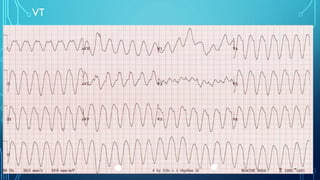
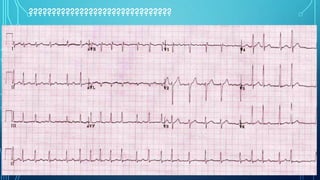
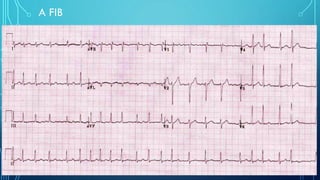
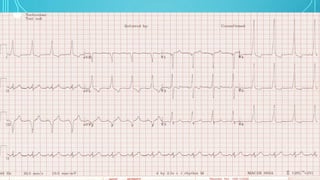
This document provides an overview of tachyarrhythmias, including their causes, clinical manifestations, and treatment approaches. It discusses various types of arrhythmias such as sinus tachycardia, atrial fibrillation, atrial flutter, premature ventricular contractions, ventricular tachycardia, and ventricular fibrillation. For each type, it outlines the etiology, characteristics, management strategies including medication and procedures. The document is an educational guide for healthcare providers on understanding and managing different cardiac arrhythmias.