This document discusses cardiac arrhythmias, including their causes, mechanisms, classification, symptoms, diagnosis and treatment. Key points include:
- Arrhythmias can occur in structurally normal hearts or those with underlying heart disease.
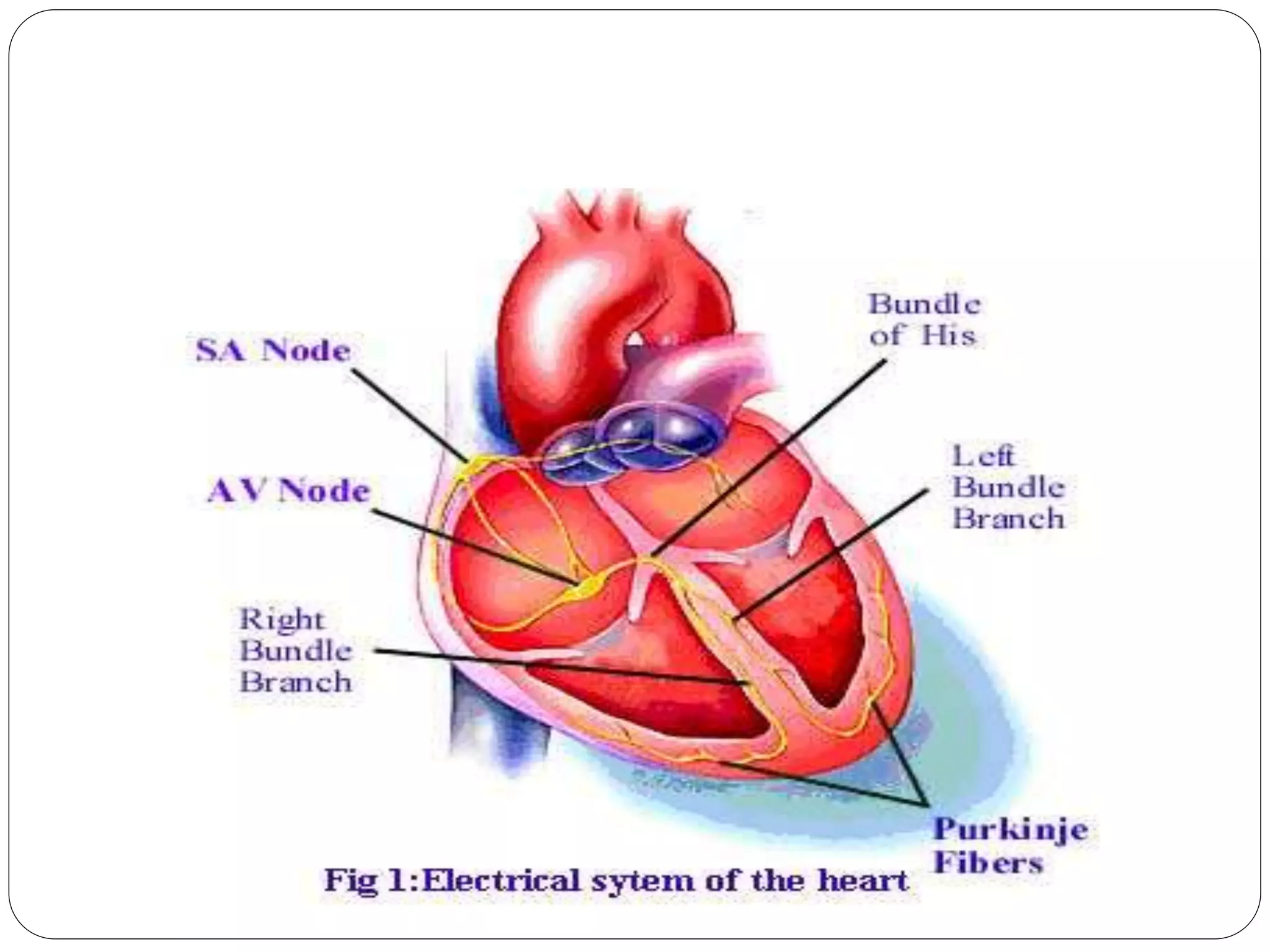
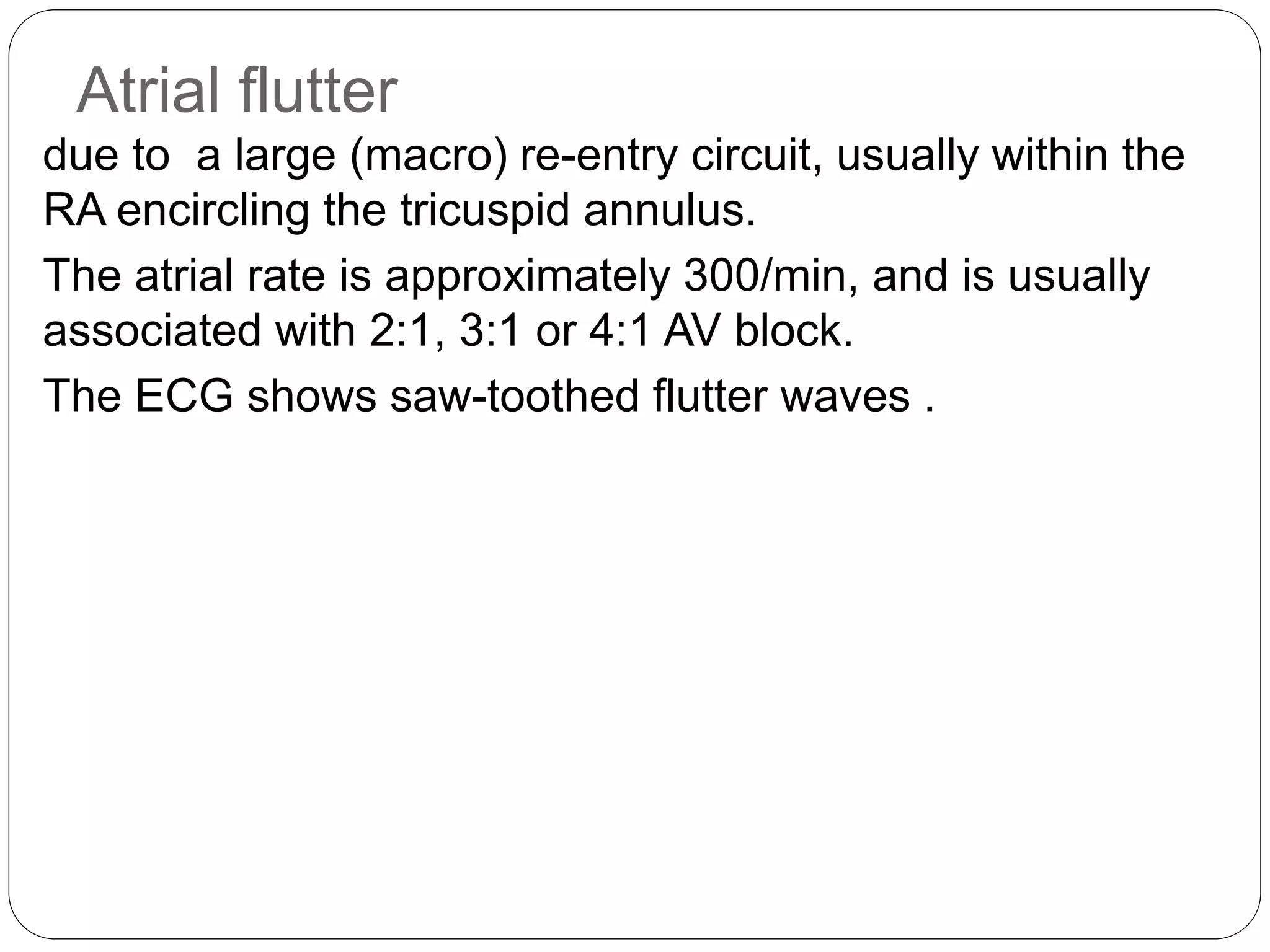
- Mechanisms include increased automaticity, re-entry and triggered activity.
- Arrhythmias are classified as supraventricular (narrow QRS) or ventricular (wide QRS).
- Common symptoms include palpitations, chest pain and fainting. ECG is used for diagnosis.
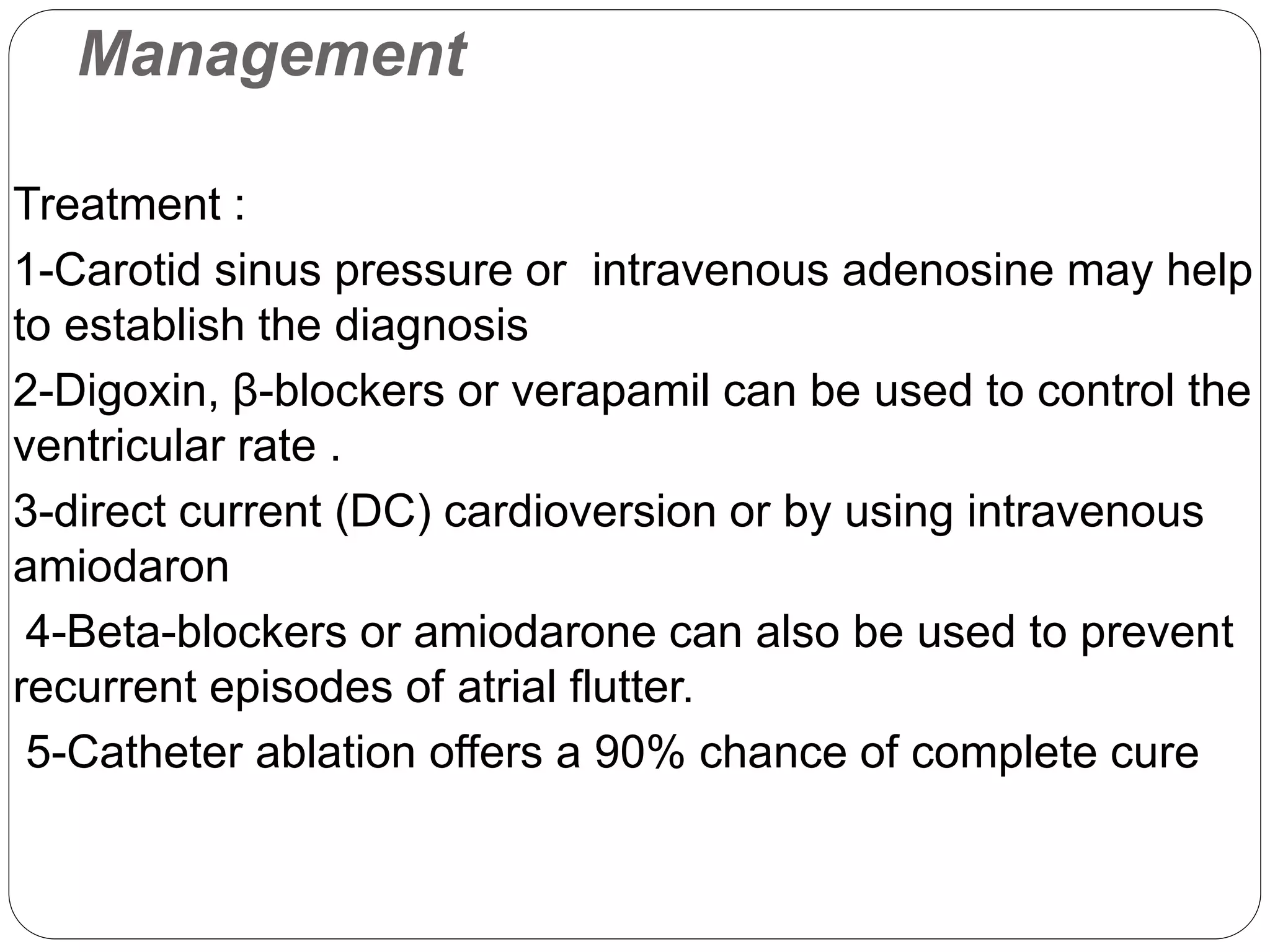
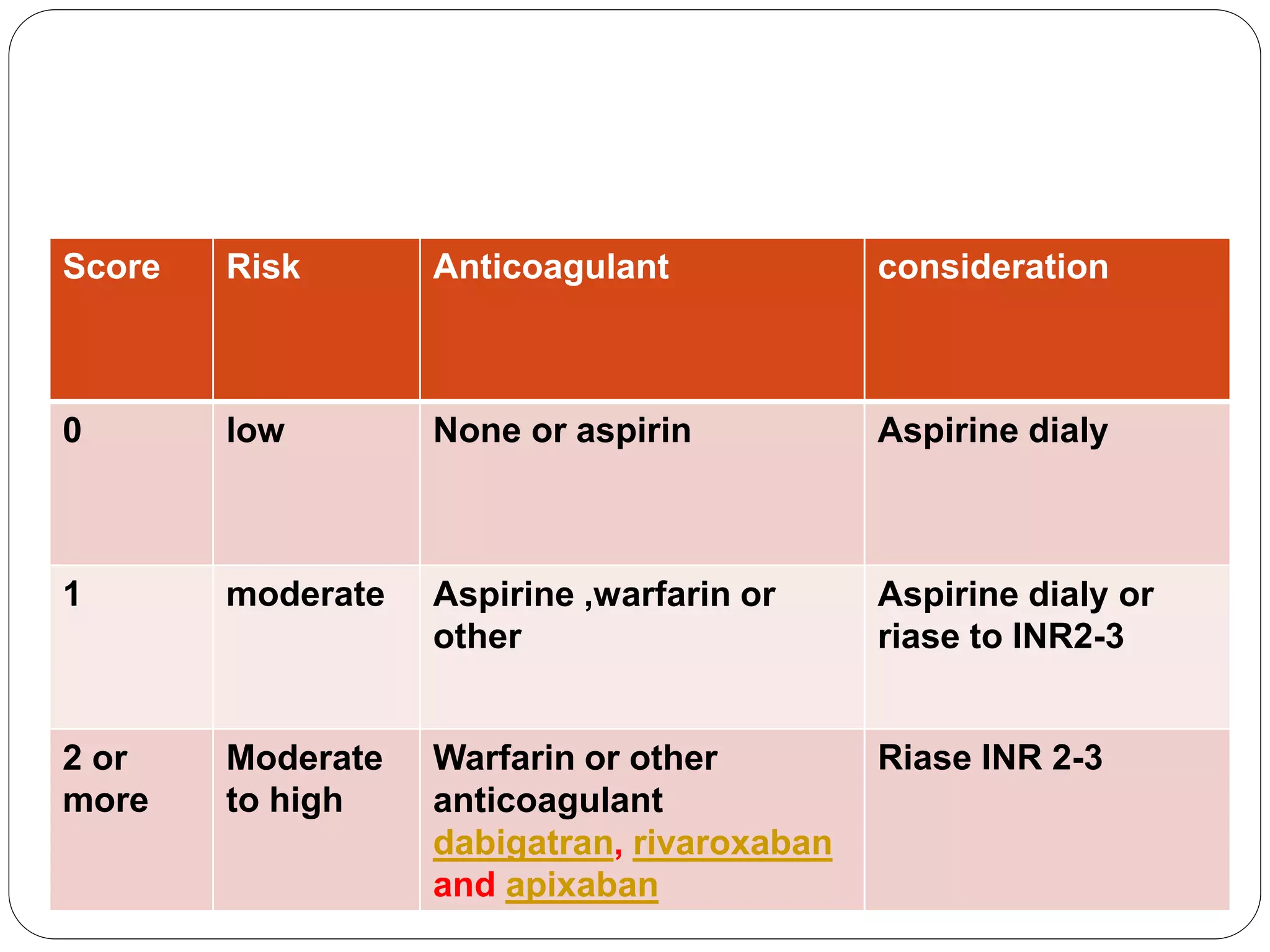
- Treatment depends on type of arrhythmia but may include medications, cardioversion, ablation, or implantable devices. Anticoagulation is often needed to prevent stroke