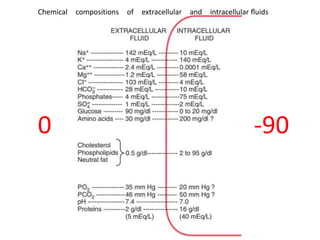
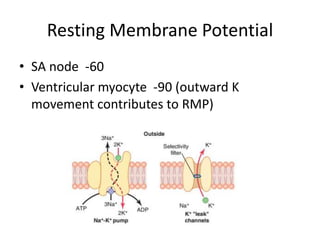
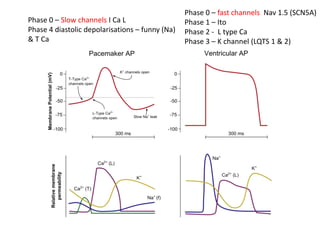
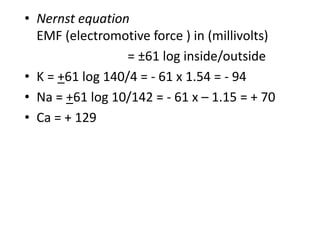
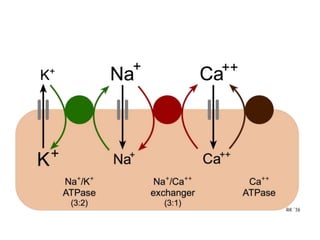
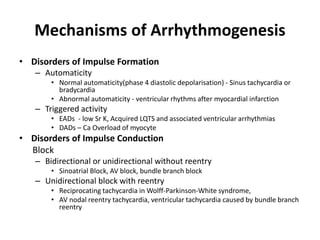
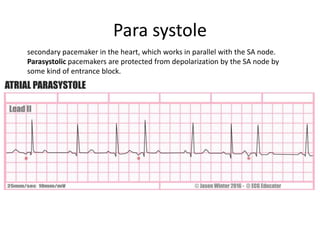
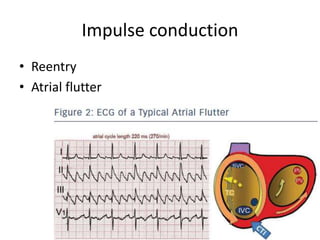
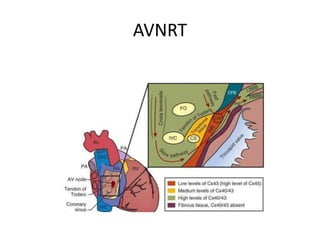
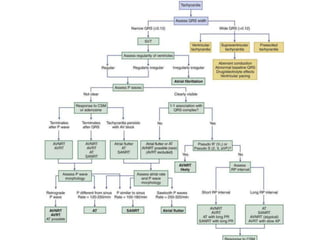
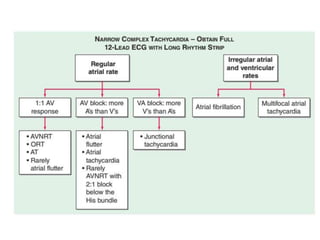
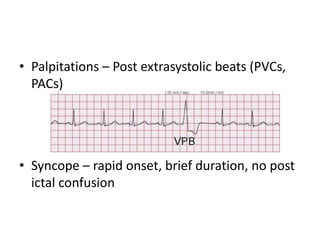
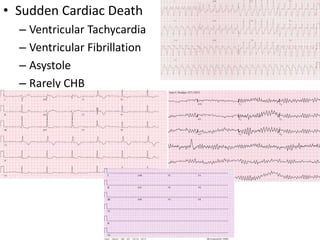
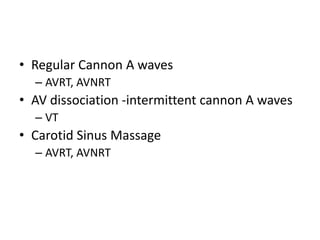
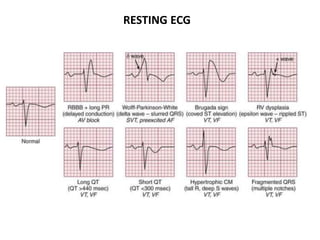
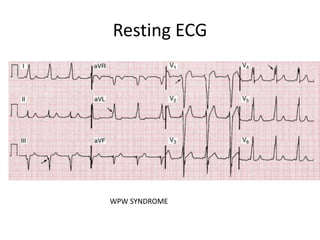
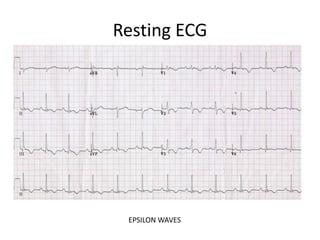
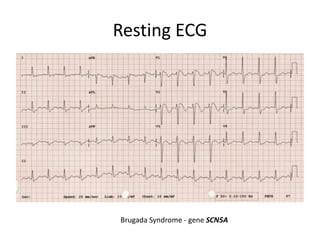
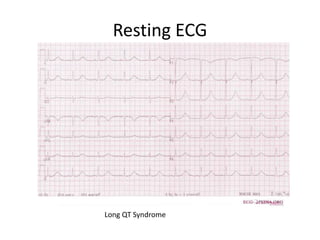
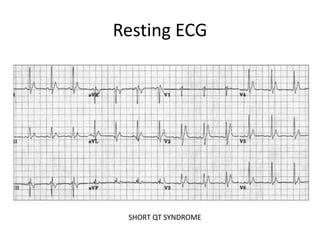
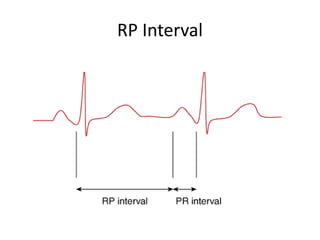
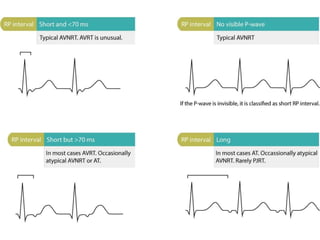
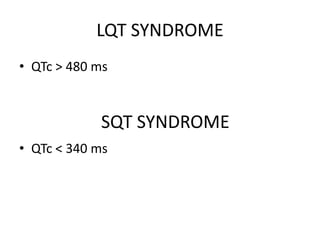
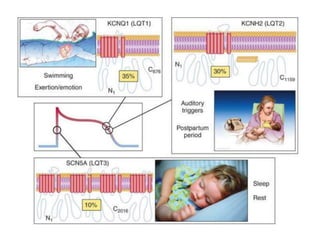
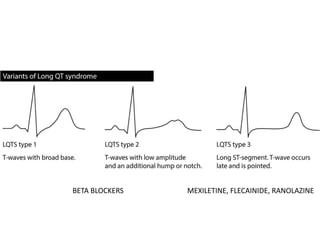
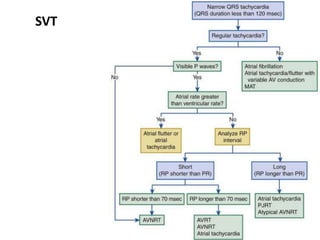
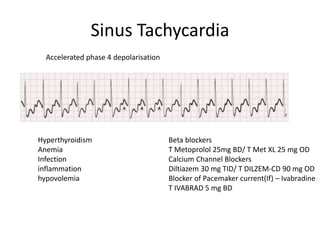
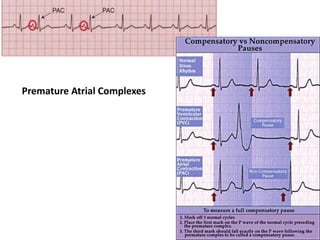
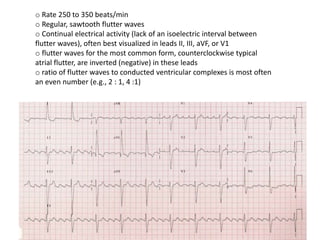
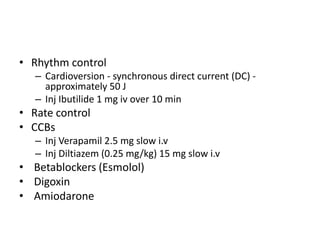
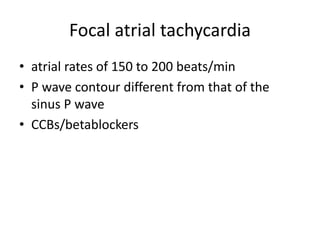
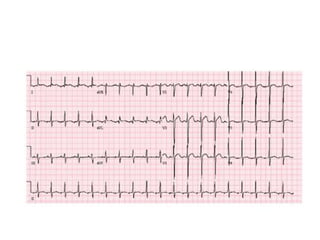
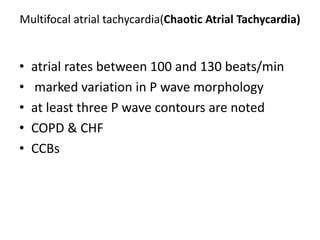
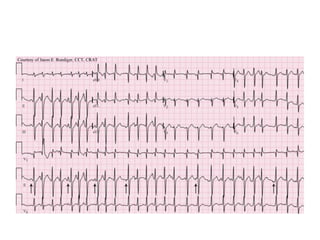
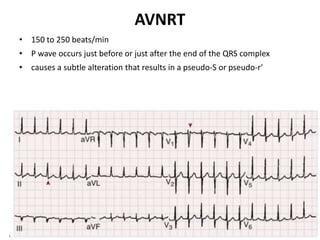
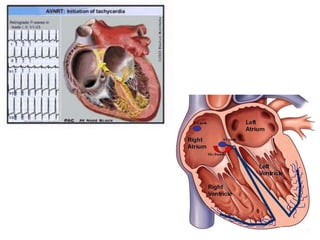
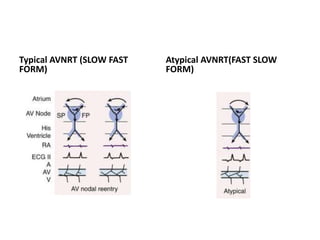
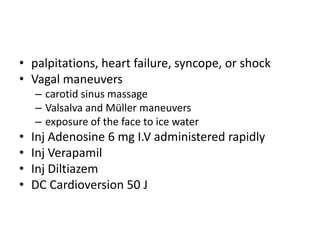
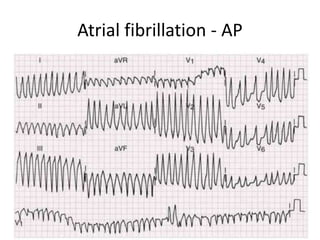
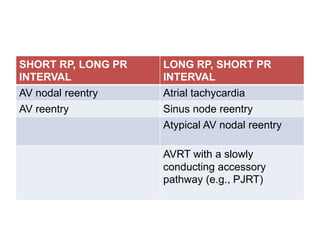
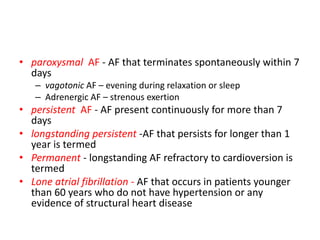
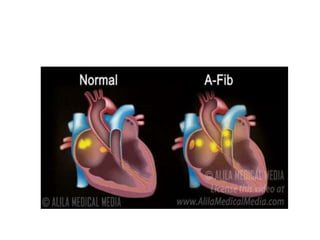
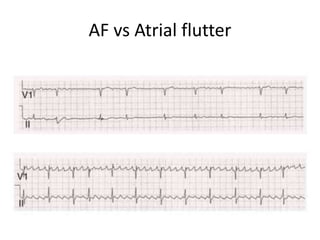
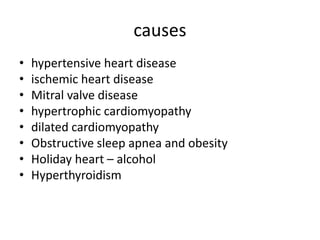
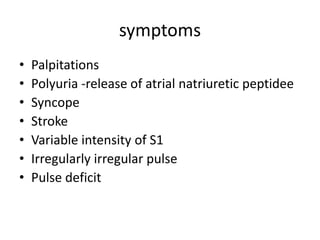
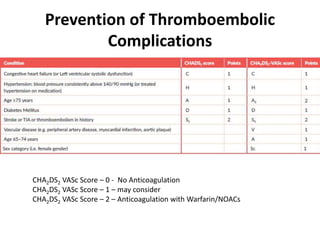
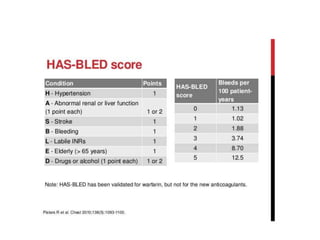
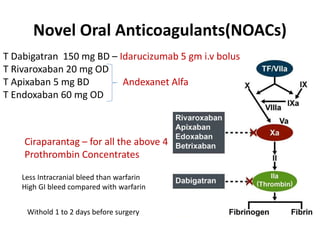
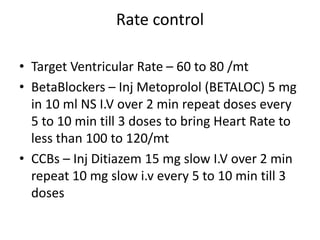
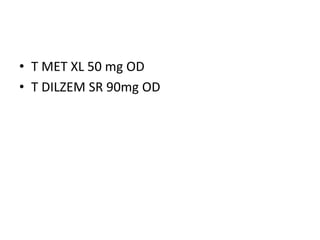
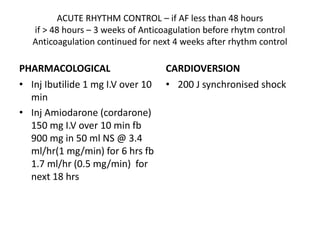
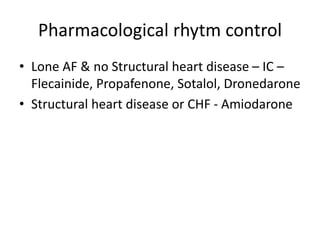
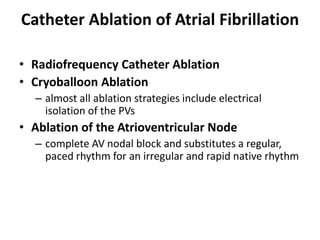
This document provides an overview of arrhythmias, including their mechanisms, types, diagnosis, and treatment. It discusses the basics of the cardiac action potential and ion channels involved. Common arrhythmias described include sinus tachycardia, premature beats, supraventricular tachycardias like AVNRT and atrial flutter, ventricular arrhythmias, and atrial fibrillation. Diagnostic tools like ECG findings and symptoms are outlined. Treatment options covered consist of medications, cardioversion, ablation procedures, and surgery.