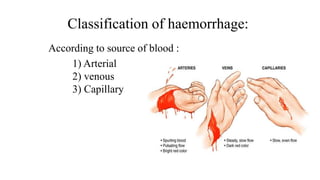
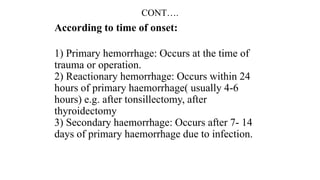
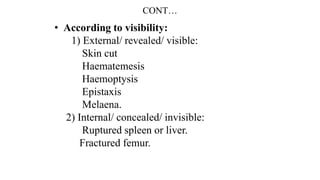
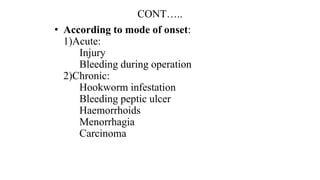
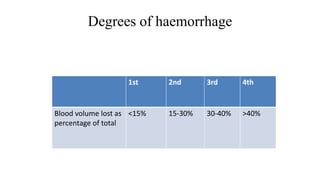
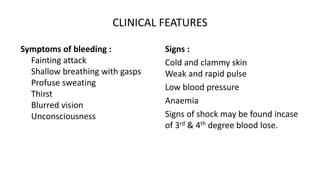
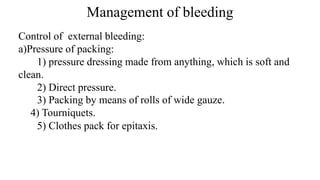
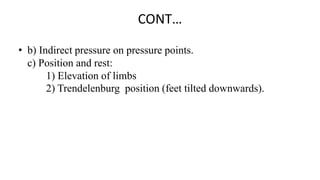
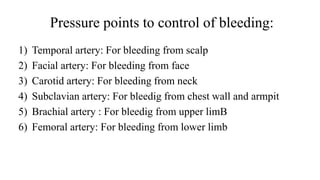
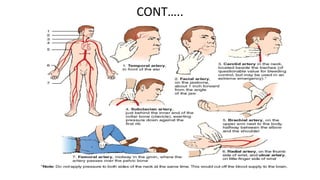
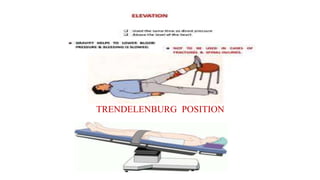
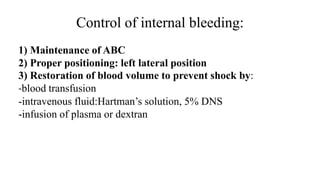
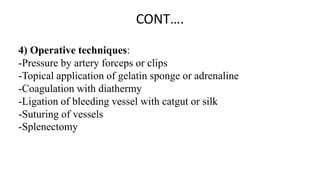
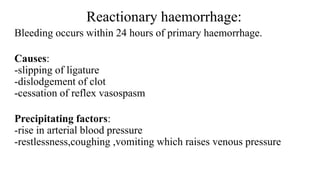
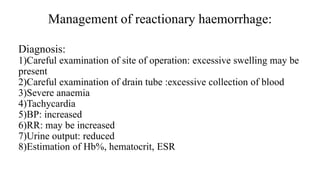
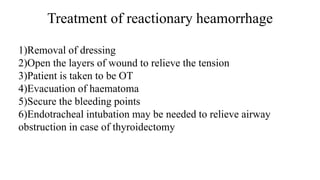
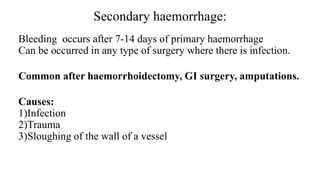
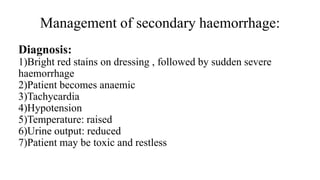
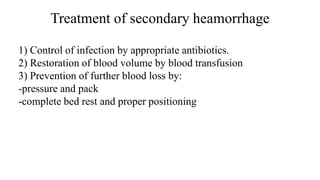
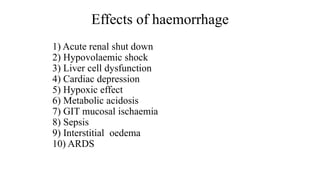
This document provides an overview of the management of bleeding. It defines hemorrhage and classifies it according to source, time of onset, visibility, and mode of onset. Reactionary hemorrhage occurs within 24 hours and secondary hemorrhage occurs 7-14 days later, often due to infection. Management involves controlling external bleeding through pressure, packing, and positioning as well as controlling internal bleeding through fluid resuscitation, operative techniques, and addressing any precipitating factors in reactionary or secondary hemorrhage. The effects of significant blood loss include shock, organ dysfunction, and metabolic derangements.