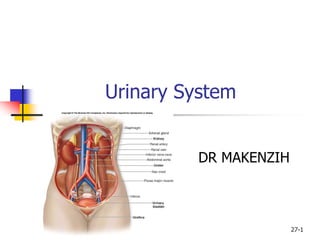
The urinary system includes the kidneys, ureters, urinary bladder, and urethra. The kidneys filter waste from the bloodstream and produce urine, which is transported via the ureters to the bladder for storage. When full, the bladder empties through the urethra. The primary functions of the urinary system are to remove waste from the blood, regulate fluid and electrolyte balance, and excrete urine.