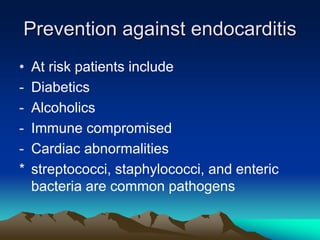
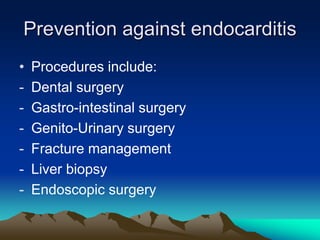
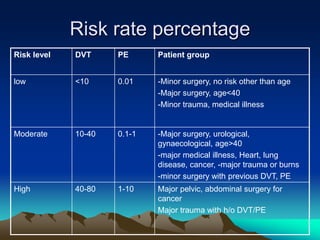
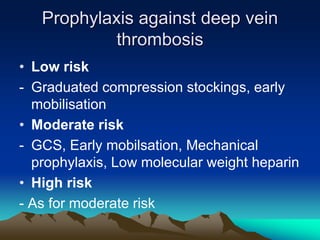
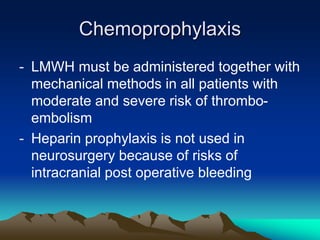
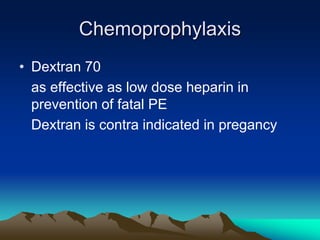
This document discusses pre-operative preparation for surgery. It defines surgery and classifies operations as elective or emergency. Elective surgeries are planned in advance. Pre-operative care involves assessing operative risk, obtaining informed consent, and correcting nutritional, fluid, electrolyte and infection deficiencies. Risk assessment aims to reduce harm to patients. Prophylactic measures prevent infections like endocarditis and surgical site infections as well as deep vein thrombosis and renal failure. Antibiotics, compression stockings, and blood thinners are used for prophylaxis depending on a patient's risk level. Thorough pre-operative preparation improves surgical outcomes and reduces morbidity and mortality.