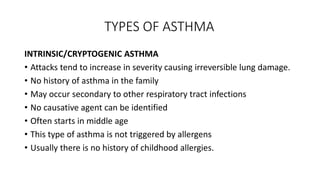
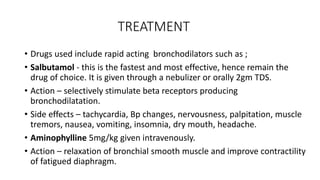
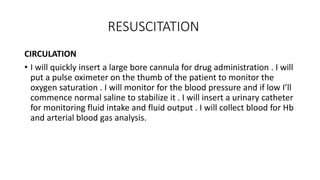
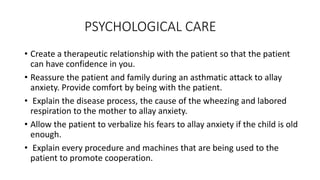
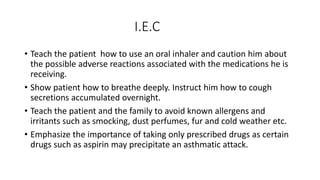
Asthma is a chronic respiratory condition characterized by inflammation of the airways causing symptoms like coughing, wheezing, and shortness of breath. It can be triggered by allergens, infections, pollution, and other factors. There are two main types - intrinsic asthma which has no identifiable cause and extrinsic asthma triggered by allergies. Treatment involves bronchodilators to open airways, corticosteroids to reduce inflammation, oxygen therapy, and avoiding triggers. Nursing care focuses on maintaining a clear airway, administering medications, monitoring for complications, and providing education to patients and families.