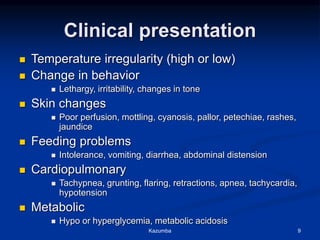
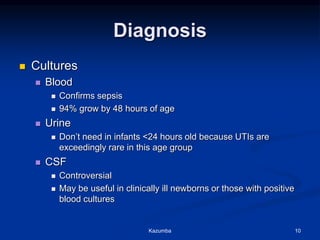
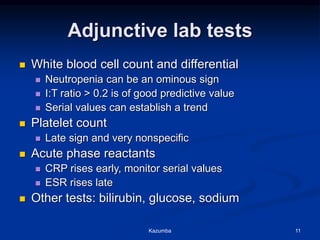
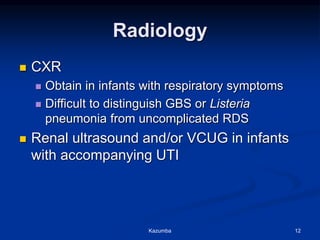
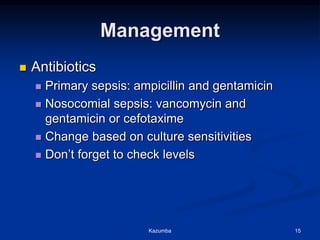
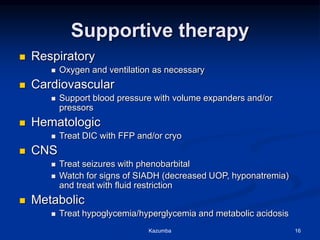
This document discusses neonatal sepsis, including its definition, incidence, causative organisms, risk factors, clinical presentation, diagnosis, management, and prevention. Neonatal sepsis can be early-onset within the first week of life, usually resulting from exposure to infected amniotic fluid or maternal genital tract bacteria during birth. Late-onset sepsis typically occurs after the first week and often has an identifiable source of infection. Prematurity and low birth weight are major risk factors. Diagnosis involves blood and other cultures with supportive lab tests. Treatment consists of antibiotics targeted to likely organisms and supportive care measures.