- Pertussis (whooping cough) is caused by the bacteria Bordetella pertussis and is highly contagious, spreading through respiratory droplets. It causes severe coughing fits that can last for months.
- The disease occurs in three stages - an initial catarrhal stage with mild symptoms, followed by weeks of intense paroxysmal coughing fits (the signature "whoop" occurs during this stage), and finally a convalescent stage as symptoms improve.
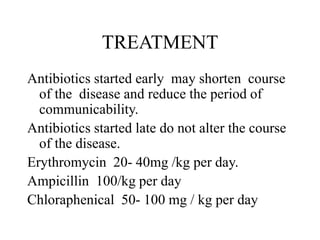
- Complications can include pneumonia, malnutrition from inability to eat during coughing fits, and long-term bronchial damage in severe cases. Treatment focuses on antibiotics, supportive care, and prevention through vaccination.