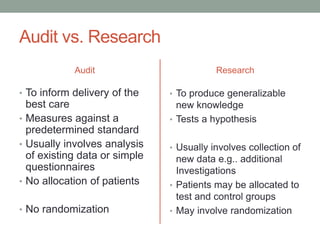
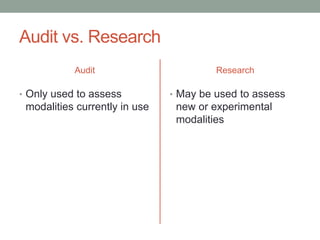
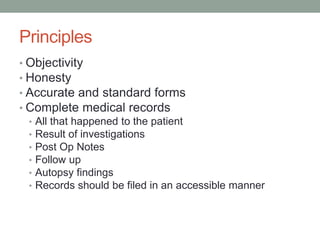
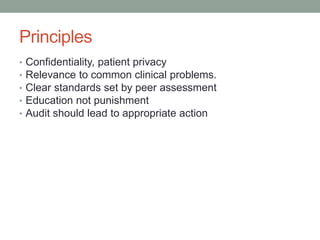
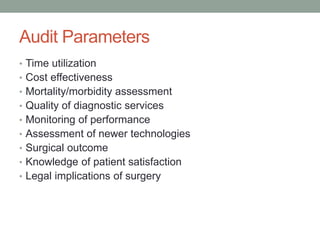
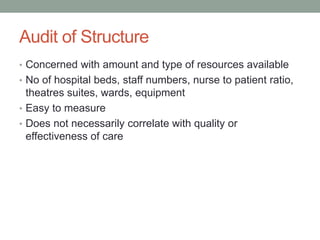
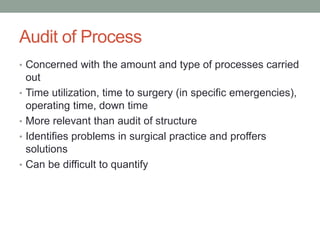
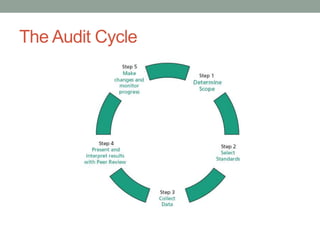
Surgical audit is a process that systematically analyzes surgical care quality against standards to improve patient outcomes. It involves collecting data on parameters like mortality, complications and outcomes and comparing results to peers to identify areas for improvement. The goal is continuous quality improvement through a non-punitive, educational process. Surgical audit has existed for centuries but modern methods began in the early 1900s and involve retrospective review of existing data to guide practice changes.